Lead Poisoning: Causes, Symptoms, Diagnosis, and Treatment
Lead poisoning is a silent enemy that has remained with us despite great victories for the environment over the last few decades. One of the sneakiest things about lead is that it quite successfully mimics certain vital minerals, so brain dysfunction, blood disorders, and renal diseases go rather unnoticed for some time.
For the NEET PG exam candidates, plumbism is a high-yielding topic in toxicology, which is well known for its classic type of presentation and very straightforward treatment regimens. This guide covers lead poisoning symptoms, causes, diagnosis, treatment, and other crucial aspects.
Keep scrolling!
What is Lead Poisoning?
Lead poisoning is a toxic condition that results from the accumulation of lead in a person’s body over time, mostly due to long-term environmental, occupational, or household exposure. Lead imitates the qualities of minerals that are essential for the body, like calcium, iron, and zinc, and thus it interferes with the enzymatic pathways, the nervous system, blood formation, kidneys, and brain development of the affected individual (usually children).
Lead poisoning, or plumbism, is one such clinical condition that is toxic in nature and is the result of the gradual buildup of lead (Pb) in the human body. It is a case of long-term exposure to environmental, workplace, or household sources of lead, like lead-based paint, drinking water, batteries, and cosmetics.
Lead is a divalent metal that has a very close similarity to the three essential minerals, namely calcium, iron, and zinc. For this reason, it competes with these ions in biological pathways, thus disrupting multiple enzyme systems and impairing cellular functions.
After lead absorption, it is carried to the brain, peripheral nerves, bones, blood, liver, and kidneys, where it interferes with neurotransmission, inhibits heme synthesis, and damages renal tubules. Most of its symptoms originate from the nervous system, and neurotoxicity is one of the features that the organ system expresses most distinctly.
Children are highly vulnerable, as they absorb lead more readily through the gut and their blood-brain barriers are still immature. Even minimal exposure may cause permanent cognitive deficits, behavioural changes, and developmental delays.
What are the Causes of Lead Poisoning?
Lead exposure is usually a result of existing surroundings, routine activities, and certain workplaces. It is very important to understand these common sources to be able to intervene early and reduce the risk of chronic harm.
Here are the common causes of lead poisoning:
- Occupational Exposure
Workplaces engaged in battery production, smelting, plumbing, printing presses, and cable production, and the paint industry prominently involve lead-containing materials. The prolonged inhalation of fumes or dust is the primary mode of exposure for people who work in such industries, making them the group at the highest risk and accounting for the largest number of cases.
- Household Sources
There might be lead-based paints in older homes, which, as they crumble, release lead-containing dust. The presence of lead may also be inferred from the use of old plumbing systems, soldered household items, children’s toys, and traditional cosmetics such as surma/kohl. People are daily exposed to these things, and such exposure usually goes unnoticed.
- Food and Water Contamination
Lead can go to the food if it’s stored in a lead-soldered can or kept in a traditional lead container or on ceramics that are not properly glazed. The release of heavy metals from contaminated groundwater is likewise a major cause of lead intake in the human body over time, especially if the area is going through industrialisation or mining.
- Traditional Practices
Some Ayurvedic or herbal medicines might deliberately contain heavy metals such as lead or be contaminated as a result of pollution. Moreover, certain generational heritage-based folk remedies that have been passed down throughout the years may also be the source of your unnoticeable exposure.
- Environmental Pollution
The lead components of the industrial waste, petrol residues, and other such leftover material may finally settle on the ground (on soil and/or crops). Thus, children playing in lead-contaminated soils and people living near industrial areas are the ones who are mostly at risk.
What are the Risk Factors of Lead Poisoning?
Certain groups and living conditions may raise the chances of lead absorption and toxicity to a great extent. Knowing the risk factors associated with it is helpful for prioritising screening and preventive measures for the most affected people.
Now, let’s see the risk factors of lead poisoning:
- Young Children Aged Between 1 and 6: Kids at an early age habitually put all kinds of things in their mouths, and their nervous systems are still in the process of development; therefore, they are the most susceptible to even small amounts of lead taken from dust, paint chips, soil, toys, etc.
- Pregnant Women: Lead is one of the harmful substances that the placenta does not filter out as it reaches the foetal development stage. If a mother has lead in her bones, which is stored from earlier exposures, the lead may be released during pregnancy, thus increasing the risks of miscarriage, preterm birth, developmental deficits, and other problems.
- Poor Nutrition: When one is iron, calcium, or zinc deficient, the lead absorption through the gastrointestinal tract increases. Malnourished people have a greater chance of being exposed to a higher level of the toxin.
- Living in Older Houses with Lead Paint: The homes that were built before the regulations that limit the use of lead were put in place are likely to have been painted with lead-based paints. Such paint may deteriorate, especially during renovations, thus creating dust that is contaminated with lead and can easily be inhaled or ingested.
- Workers Without Adequate Safety Measures: People engaged in roles such as battery factories, smelting units, construction, painting, or cable manufacturing may be exposed to lead dust and fumes. Lack of protective equipment or improper use significantly escalates their risk.
What are the Symptoms of Lead Poisoning?
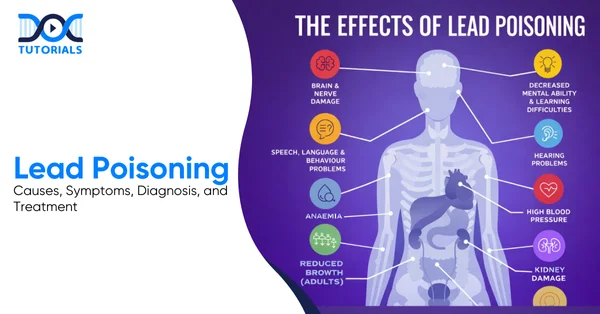
Lead toxicity produces a very diverse range of clinical manifestations as the metal builds up in different organs of the body over time. The intensity and signs of the condition vary according to the dose, time of exposure, and the patient’s age.
- Neurological Symptoms
When lead interferes with neurotransmission and injures both central and peripheral nervous structures, it results in behavioural, cognitive, and motor control changes:
- Irritability and Behaviour Changes: Behavioural changes associated with neurotoxicity are illustrated by mood changes, hyperactivity, shortened attention span, and social withdrawal, especially in children.
- Cognitive Decline and Poor Concentration: Lead interferes with synaptic formation and neural signalling, which causes difficulties in learning, memory, and concentration.
- Peripheral Neuropathy (wrist drop, foot drop): Over time, motor nerves are damaged due to chronic exposure; thus, weakness of the extensor muscles and the development of typical nerve palsies occur.
- Encephalopathy: Headache, vomiting, seizures, and altered sensorium are some of the symptoms of lead toxicity, along with increased intracranial pressure, and it may even progress to coma if not treated.
- Gastrointestinal Symptoms
These symptoms appear when lead stops the function of smooth muscles in the digestive tract and inflames the gastrointestinal mucosa, which is why the patient experiences continuous digestive discomfort.
- Lead Colic (severe abdominal pain): A typical case involves extremely severe, cramping pain caused by spasm of intestinal smooth muscle.
- Constipation, Anorexia, Vomiting: Difficulty in bowel movements, vomiting, and loss of appetite occur as digestive tract motility gradually decreases.
- Metallic Taste, Weight Loss: Changed taste sensation leads to less food intake and slow weight loss.
- Haematological Symptoms
They happen because lead inhibits the key enzymes of heme synthesis and disturbs red blood cell maturation, which eventually leads to defective erythropoiesis.
- Microcytic Hypochromic Anaemia: The failure of heme production causes the blood cells to be small and pale, which means the oxygen-carrying capacity of the cells is lowered.
- Basophilic Stippling of RBCs: Yet another diagnostic sign is the presence of typical coarse granules in the blood cells due to impaired RNA degradation.
- Fatigue, Pallor: The reduction of haemoglobin causes the patient to feel tired all the time, experience a lack of energy during physical activities, and see the skin and mucous membranes becoming pale.
- Renal and Musculoskeletal Effects
These symptoms are a result of damage to renal tubules due to chronic lead buildup in the kidneys and deposition in bones and joints, thus causing metabolic and structural changes. They include:
- Interstitial Nephritis: The kidney damage caused by lead in the tubules is the main reason for renal filtration impairment, proteinuria, and gradual kidney failure.
- Hyperuricemia (“saturnine gout”): Decreased uric acid excretion causes increased serum urate levels, resulting in joint inflammation similar to gout.
How is Lead Poisoning Diagnosed?
Diagnosis of lead poisoning is based on a mixture of lab tests, imaging results, and probes that help figure out how deeply the patient has been poisoned and how many organs have been affected.
- Laboratory Findings
The tests mentioned here directly detect lead levels in the blood and reveal typical haematological changes due to impaired heme synthesis.
- Blood Lead Level (BLL):
- 5 g/dL: Points to exposure to a worrying level, and the source needs to be evaluated.
- 45 g/dL: In such a case, where a patient is showing symptoms, the use of chelation therapy is advised.
- 70 g/dL: A medical emergency is signalled because of the risk of severe neurological damage.
- Zinc Protoporphyrin (ZPP): An elevated ZPP level reflects the concept of inhibited heme synthesis and aligns with the idea of chronic lead exposure.
- Free Erythrocyte Protoporphyrin Raised: A marker of heme production disruption, most of the time it is at a high level before the onset of anaemia.
- CBC Reveals Microcytic Anaemia with Basophilic Stippling: A peripheral smear shows small, pale RBCs and coarse granules, both of which are the typical features of lead toxicity.
- Imaging
Radiological studies serve the purpose of locating lead-induced changes in the skeletal system, helping clinicians, especially with diagnoses of children suffering from long-term lead exposure.
- Children’s Radiographs: May show thickened metaphyseal lead lines at growth plates, which are areas where lead has been accumulated for a long time in bones.
- Additional Tests
The aim here is to determine how well the organs work and to keep an eye on the excretion process of lead during treatment and after it has finished.
- Renal Function Tests: For the evaluation of kidney damage that can be a consequence of chronic tubular injury.
- Urine Lead Levels (post-chelation): It is a measurement taken after chelation therapy to evaluate the amount of lead that is being released and excreted.
What are the Treatment Options for Lead Poisoning?
Lead poisoning management largely depends on removing the patient from the lead source, stabilising their condition, limiting lead absorption, and finally chelating the lead.
Let’s take a look at the first line and supportive treatment options for lead poisoning:
- Immediate Measures
These measures remove the patient from the lead source as fast as possible and stabilise the patient’s physiology to prevent further damage:
- Remove Patient from Exposure Source: Immediate stopping of the patient’s contact with the occupational, environmental, or household source is the very first and most vital step.
- Rehydrate and Maintain Nutrition: Proper hydration and dietary intake (particularly iron and calcium) will not only lower lead absorption but also be supportive of the general recovery process.
- Lead Poisoning Antidotes (Chelating Agents)
| Drug | Indication | Key Notes |
| EDTA (Calcium Disodium EDTA) | Moderate-severe toxicity | IV: May cause nephrotoxicity |
| Dimercaprol (BAL) | Severe toxicity, especially with encephalopathy | Often combined with EDTA for severe cases |
| D-Penicillamine | Mild-moderate chronic poisoning | Oral: Used for long-term therapy |
| Succimer (DMSA) | Preferred in children | Oral: Well-tolerated |
- Supportive Care
Supportive treatment deals with the complications of lead poisoning in the nervous system, blood, and kidneys, and also prepares the patient for chelation therapy, which may be required.
- Control of Seizures in Encephalopathy: Seizures associated with lead intoxication can be controlled with the administration of benzodiazepines or other anticonvulsants.
- Treatment of Anaemia: Iron therapy or transfusion may be necessary to correct microcytic anaemia that is caused by the inhibition of the heme synthesis pathway.
- Monitoring of Renal Function: It should be regularly monitored because long-term lead exposure may lead to renal tubular dysfunction, and this is a very common side effect of chelation therapy.
What are the Complications of Untreated Lead Poisoning?
When lead poisoning persists for a prolonged period without treatment, the metal builds up in the body and causes permanent damage, in many cases, organ failures as well. Children remain the most vulnerable to this condition, as their bodies absorb more lead when their nervous systems are still in the development phase.
Below is a detailed discussion on the complications caused by untreated lead poisoning:
- Permanent Cognitive Impairment in Children: Chronic lead exposure alters synaptic development and neuronal maturation, resulting in permanent decreases of IQ, learning ability, attention, and behaviour.
- Developmental Delay: Infants and young children may be less mobile, have delayed speech, show less interest in social interaction, and have impaired cognitive functioning.
- Chronic Nephropathy: The tubular injury caused by lead can evolve into interstitial nephritis, a urine concentrating defect, proteinuria, and eventually chronic kidney disease.
- Infertility and Miscarriage: Lead impairs reproductive hormones, damages gametes, and crosses the placenta; the risks of miscarriage, preterm birth, and decreased fertility in both men and women are elevated.
- Peripheral Neuropathy: Exposure over a long period damages peripheral nerves, thus the patient experiences motor weakness, sensory deficits, and typical wrist or foot drop.
- Stunted Growth: Lead disrupts bone metabolism and endocrine regulation; thus, children who are chronically exposed have reduced height growth.
- Cardiovascular Hypertension due to Renal Damage: Chronic nephropathy changes renin-angiotensin regulation and causes vasoconstriction, thus leading to persistent hypertension.
How to Prevent Lead Poisoning?
Preventing lead poisoning involves different layers of strategies that focus on the root causes in homes, workplaces, and nature. Moreover, early testing and public health interventions are essential in lessening the risk, particularly to sensitive groups like kids and expectant mothers.
The following actions aim to eliminate or at least minimise lead exposure from the daily environment, the workplace, and the community:
- The inspection of homes, especially old buildings, for deteriorated lead-based paint is a must, as the dust coming off the paint is nowadays the main source of lead exposure.
- Children should be discouraged from playing in the ground near roads, old buildings, and industries, which are always areas of lead deposition.
- Children within the age bracket of 1 to 5 years should have their blood lead levels checked regularly, especially if they reside in an old house or a contaminated area.
- The use of personal protective equipment and safety procedures by workers in industries such as battery manufacturing, smelting, and construction is a must.
- Lead pipes, solder, and fixtures are the main culprits of lead in drinking water that develops in most cases over a long period of time. So, the replacement of these parts with lead-free ones greatly contributes to the prevention of prolonged consumption, especially in old houses and public buildings.
- Disposal of industrial waste in an environmentally friendly manner is not only good for the planet but also for the health of people living nearby.
FAQs about Lead Poisoning
1. What’s the most common symptom of lead poisoning in children?
Children with lead poisoning usually show crankiness, fall behind in their development, experience abdominal pain, and have difficulties in learning.
2. What’s the antidote for lead poisoning?
Doctors use chelating agents like EDTA, BAL, DMSA (succimer), or D-penicillamine to treat lead poisoning. The selection of an antidote depends on the severity of the symptoms.
3. How do you diagnose plumbism?
To diagnose plumbism, you need to check blood lead levels, run a CBC and ZPP, and sometimes rely on radiological findings.
4. Can you reverse lead poisoning?
Neurological damage may be irreversible, especially in children. Diagnosing it early and treating it fast significantly improves outcomes.
5. Who’s most at risk for lead poisoning?
Children, pregnant women, and anyone working in industries dealing with batteries, paint, smelting, or manufacturing face the highest risk of lead poisoning.
Conclusion
Lead poisoning is usually thought of as a toxicological curiosity from the past, but in reality, it remains an active clinical and public health problem. It retains equal importance for NEET PG candidates. Aetiology, symptomatology, diagnosis, and treatment based on proof are highly relevant toward fetching good marks in the examination paper and identifying actual cases where treatment can make a difference.
DocTutorials assists students who intend to prepare basic and conceptual knowledge about Forensic Medicine through organised learning and preparation for exams. Lead poisoning is a high-yield topic because it is continuously asked in entrance examinations.
Instead of cramming notes, understanding the concept with our video lectures and expert guidance will ensure long-term memory retention and application in real scenarios with confidence.
Check out our NEET PG courses today!
| > Bed Sores | > Pruritus |
| > Polycythemia Vera | > Corticosteroids |
| > Biomedical Waste Management | > Hot Flashes |
| > Tinea Versicolor | > Xerostomia |
| > Kwashiorkor | > Narcolepsy |
Latest Blogs
-

NEET PG Exam 2025- Date, Pattern, Marking Scheme, Subject Wise Weightage, and Exam Mode
NEET PG Exam 2025 is the ultimate gateway for medical graduates aspiring to pursue postgraduate courses in medicine, including MD,…
-

INI CET Exam 2025: Your Roadmap to Success – Key Topics, Strategies, and Lessons from Last Year’s Papers
The INI CET exam is more than just a test; it’s a significant milestone for many medical students aiming to…
-

INI CET Exam Success: Previous Year Question Papers & Ultimate Guide – INI CET PYQ
One can feel overwhelmed while preparing for the INI CET (Institute of National Importance Combined Entrance Test). A vast syllabus,…





