Necrotising Enterocolitis: Causes, Risk Factors, Symptoms, Diagnosis, and Treatment Options
Necrotising enterocolitis (NEC) refers to a gastrointestinal emergency that is common in preterm neonates in the NICU. Some infants experience mild NEC, while others can experience life-threatening severe symptoms. NEC can also occur in term babies who are born with asphyxia, heart disease, polycythaemia, sepsis, and hypotension.
Necrotising enterocolitis is a crucial and high-yielding topic for NEET-PG aspirants and can help you achieve a good score in the NEET-PG exam. In this guide, we are going to cover all the information about necrotising enterocolitis, including causes and risk factors, symptoms and diagnosis, treatment options, and other crucial aspects.
Keep reading to learn more!
What is Necrotising Enterocolitis?
NEC is a common gastrointestinal condition in premature babies and can lead to perforations as well. Babies with low birth weight and those fed enterally have a higher risk of developing this condition. It can be life-threatening if left untreated.
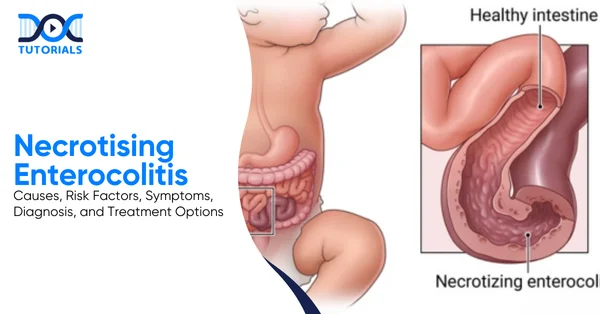
Necrotising enterocolitis is a neonatal gastrointestinal disorder characterised by ischaemic and inflammatory necrosis of the intestinal wall, leading to systemic sepsis and potential perforation.
Necrotising enterocolitis is a common disease in premature babies. Almost 90% of all babies who suffer from NEC are premature babies. The incidence of NEC is about 1 in 1000 premature babies. Moreover, low birth weight babies and enterally fed babies are at a higher risk of developing necrotising enterocolitis.
What are the Causes and Risk Factors Involved?
As of now, the exact cause of necrotising enterocolitis is not known. Healthcare providers usually link this condition to the underdeveloped immunity and circulatory systems of premature babies, which provide an ideal environment for intestinal pathogens to affect the intestines. Major causes include premature birth, low birth weight, term babies born with asphyxia or heart disease, etc.
The exact cause of necrotising enterocolitis is not yet known. However, healthcare providers believe it is due to the underdeveloped immunity of the premature babies. The immune system takes a long time to develop to its full potential, usually crossing infancy and childhood.
This gives the intestinal pathogens an opportunity to infest the intestines. Since the immunity is underdeveloped, the body faces a harder time fighting the pathogens.
Moreover, the circulatory system of a premature baby is not fully effective. This deters the flow of blood to the intestines, leading to a decreased extent of the immunoglobulins and ischaemic damage to the intestines.
What are the Major Risk Factors of Necrotising Enterocolitis?
The risk factors of necrotising enterocolitis do not cause the disease directly, but make it more likely to develop:
- Prematurity is the most consistent risk factor
- Hypoxic-ischaemic injury leading to gut ischaemia and inflammation
- Enteral feeding
- Lack of breastfeeding
- Use of acid suppression drugs
- Patent ductus arteriosus
- Term babies born with asphyxia, heart disease, polycythaemia, sepsis, and hypotension
- Low birthweight babies
What are the Symptoms and Diagnostic Modalities for NEC?
NEC has both systemic and GI manifestations, and the course can be very rapidly progressive. Clinical symptoms generally include feeding intolerance and increased gastric residuals, with bloody stools, lethargy, and abdominal wall erythema being the advanced symptoms. Diagnostic methods generally include lab tests and radiological diagnosis.
Clinical Features
The clinical features, including signs and symptoms for NEC, are tabulated below:
| Early symptoms | – Feeding intolerance- Increased gastric residuals- Abdominal distension- Vomiting |
| Advanced symptoms | – Bloody stools- Abdominal wall erythema- Apnoea and bradycardia- Lethargy- Temperature instability- Shock in severe cases |
| Physical Examination | – Tense, distended abdomen- Decreasing bowel sounds- Abdominal tenderness- Palpable abdominal mass (late) |
Diagnostic Testing
| Laboratory Findings | – Thrombocytopenia- Metabolic acidosis- Leukocytosis or leukopenia- Increased levels of C-reactive protein |
| Radiological Diagnosis (Cornerstone) | – Abdominal radiography- Pneumatosis intestinalis is pathognomonic- Portal venous gas – Dilated bowel loops – Free air under the diaphragm (perforation) |
Bell’s Staging (Essential for Examination)
Bell’s staging is used to assess the severity of necrotising enterocolitis in a newborn. This helps to decide the management for the affected baby.
| Stage | Feature |
| Stage I | Suspected NEC |
| Stage II | Definite NEC |
| Stage III | Advanced NEC with perforation |
What are the Treatment Options for NEC?
NEC can be a life-threatening condition. Hence, early diagnosis, prompt treatment, and prevention of complications can help the baby recover faster and prevent mortality. The main aims of treatment include maintenance of nutrition, clearing of the pathogenic load, and prevention of recurrence.
Your baby’s intestines need time to rest and heal. The first part of treating NEC is to stop all feedings by tube and mouth. Instead, your baby will get the fluids and nutrition he or she needs through an intravenous line (IV).
Your baby may also receive several other therapies, like:
- Nasogastric Tube
A provider gently places a long, narrow tube through the nose and sometimes through the mouth, down to the stomach, allowing removal of accumulated gas and fluids.
- Antibiotics
These help in combating bacterial infections. May include ampicillin, clindamycin, or metronidazole, and gentamicin.
- Surgery
About one quarter of babies with NEC need surgery to remove sections of dead intestinal tissue and to repair any holes. Sometimes, your baby’s provider may do an ostomy procedure. This surgery involves:
- Creation of a small opening, called a stoma, in the abdomen.
- Connecting the large intestine to the stoma.
- Allows waste to leave the body through the stoma into a bag worn outside the body.
When your baby gets a bit stronger, the intestines can be reattached and returned to their original place inside the abdomen. If your baby is tiny, less than 1 pound, or too sick for surgery right away, your provider may insert a drain or a catheter into the abdomen.
A drain can help your baby feel better sooner by draining out unhealthy and infected fluids and gas. If more surgery is needed, it will be scheduled at a later time when your baby is larger and healthier.
Prevention Methods for NEC
If you have a risk of having a premature baby, the doctors would prescribe you some corticosteroid injections. These steroids help in boosting the foetus’s development, thus reducing the chances of intestinal or lung issues.
Also, initiating early breastfeeding in a baby helps to develop their immune system. The breast milk contains a lot of essential immunoglobulins, which help your baby develop their passive immune system.
FAQs about Necrotising Enterocolitis (NEC)
- What is the major causative factor of NEC?
While the exact causes of NEC are not yet known, it generally occurs in premature infants, whose underdeveloped intestinal and circulatory systems create an ideal environment for intestinal pathogens.
- What is the treatment modality for NEC?
Treatment of NEC involves supportive care, nasogastric feeding, surgical treatment, IV fluids and antibiotics, and close monitoring of the baby.
- What is the mortality rate for NEC?
The overall mortality rate for NEC usually ranges between 10% and 50%.
- What are the long-term complications of NEC?
Even after surgery, some infants can face problems like short bowel syndrome, inadequate digestion, and poor growth.
- What early signs appear in NEC?
The early signs of NEC are abdominal distension, bloody stools, poor feeding, and bilious vomiting or stools.
Conclusion
Necrotising enterocolitis is a serious disease as well as a hot topic for the NEET-PG examination. It is a high-incidence disease in newborns, especially in premature babies. It is a curable and preventable condition as well.
What is important to know about NEC is its early detection and prompt cure. To understand more in detail about NEC, and other conditions, check out DocTutorials. We offer concise and crisp video lectures, clinical Qbanks, exam-focused notes, and mind maps to aid aspirants and guide them towards a better understanding of medical concepts. Explore our NEET PG courses today!
| > Bed Sores | > Pruritus |
| > Polycythemia Vera | > Corticosteroids |
| > Biomedical Waste Management | > Hot Flashes |
| > Tinea Versicolor | > Xerostomia |
| > Kwashiorkor | > Narcolepsy |
Latest Blogs
-

NEET PG Exam 2025- Date, Pattern, Marking Scheme, Subject Wise Weightage, and Exam Mode
NEET PG Exam 2025 is the ultimate gateway for medical graduates aspiring to pursue postgraduate courses in medicine, including MD,…
-

INI CET Exam 2025: Your Roadmap to Success – Key Topics, Strategies, and Lessons from Last Year’s Papers
The INI CET exam is more than just a test; it’s a significant milestone for many medical students aiming to…
-

INI CET Exam Success: Previous Year Question Papers & Ultimate Guide – INI CET PYQ
One can feel overwhelmed while preparing for the INI CET (Institute of National Importance Combined Entrance Test). A vast syllabus,…




