Pancreatitis | Causes, Symptoms, Diagnosis, and Treatment
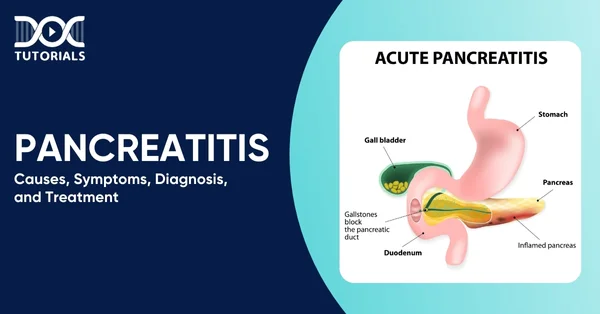
Pancreatitis is an inflammation of the pancreas, the organ located behind the stomach that plays a crucial role in digestion and blood sugar regulation. This condition can be acute (short-term and sudden) or chronic (long-term).
The acute form of the disease normally responds to treatment, whereas the chronic form tends to cause progressive damage and scarring. With the increase in the number of cases and complications, this condition has become crucial to master for the NEET PG exam.
Continue reading for a detailed insight into the types, causes, symptoms, diagnosis, and treatment of pancreatitis.
What are the Types of Pancreatitis?
Listed below are 2 main types of pancreatitis:
- Acute Pancreatitis: A rapid-onset inflammation. The majority of patients recover within several days of treatment (fluids, rest, pain relief), whereas in severe cases, complications or organ failure might occur.
- Chronic Pancreatitis: Chronic fibrosis and loss of function due to long-term inflammation. Lukewarts are recurrent or persistent, and over time, they may lead to malabsorption and diabetes.
What are the Causes and Risk Factors of Pancreatitis?
Listed below are the causes and risk factors of pancreatitis:
Causes
Gallstones and over-indulgence in alcohol are the two most prevalent causes of pancreatitis. Gallstones may block the pancreatic duct, and the digestive juices will back up into the pancreas, leading to inflammation.
Risk Factors
Risk is also significantly elevated by excessive alcohol consumption; in actual fact, nearly about 25–50% of acute cases are alcohol-related. Other risk factors are:
- Hypertriglyceridemia: Sections of the pancreas can become inflamed under high levels of blood triglycerides (usually above 1000 mg/dL).
- Hypercalcemia: Excess calcium (as in hyperparathyroidism) can activate pancreatic enzymes.
- Medications and Procedures: There are some drugs (e.g. azathioprine, valproate) and procedures which may trigger pancreatitis, such as ERCP (endoscopic retrograde cholangiopancreatography).
- Infections and Trauma: It may be provoked by some infections (mumps, hepatitis) or by a direct injury to the abdomen.
- Genetic Factors: There may be inherited mutations (e.g. in the trypsinogen gene or cystic fibrosis gene) leading to a propensity to repeated pancreatitis.
- Autoimmune Pancreatitis: A rare condition in which the body’s immune system attacks the pancreas.
Critical risk factors of pancreatitis are excessive consumption of alcohol, smoking, obesity, and high BMI (body mass index). An individual with a family history or genetic mutations is also at risk. Interestingly, in some cases, no distinct cause is identified (idiopathic pancreatitis).
What are the Symptoms of Pancreatitis?
Upper abdominal pain is the distinctive symptom of pancreatitis. Pain due to acute pancreatitis is typically abrupt and might spread directly through the abdomen into the back. The belly can be sensitive to the touch. Other general acute pancreatitis symptoms are:
- Nausea and vomiting
- Fever and rapid pulse
- Abdominal swelling and tenderness
There could be the persistence or recurrence of pain in chronic pancreatitis, and the pain usually increases following the meals. Symptoms associated with loss of the pancreatic function over time include oily stools (steatorrhea), weight loss, and diabetes.
What is the Diagnosis of Pancreatitis?
Diagnosis of pancreatitis is based on clinical signs, lab tests, and imaging. In cases of common abdominal pain, physicians examine the blood for the presence of pancreatic enzymes. An elevated lipase or amylase (three times normal) is a strong predictor of acute pancreatitis, and lipase is more specific and takes a long period to subside.
Imaging can assist in diagnosing the condition and seeking causes and complications:
- Abdominal Ultrasound: Usually done initially to check for gallstones or blockage of the ducts.
- CT (computed tomography) Scan: Can help to see the presence of pancreatic inflammation, size of swelling or necrosis; helpful in cases of uncertain diagnosis or non-improving patients.
- MRI (magnetic resonance imaging): It has the ability to demonstrate pancreatic inflammation and anatomy of the duct without radiation.
In chronic pancreatitis, enzyme loss is assessed by tests such as stool elastase, and diabetes is screened by glucose tolerance. Organ functioning and inflammation are also assessed by means of blood tests.
What are the Treatment Options for Pancreatitis?
Effective pancreatitis treatment is effective based on the type and severity of the condition.
Treatment for Acute Pancreatitis
The treatment of acute pancreatitis patients is mainly supportive, as follows:
- Hospital Admission with IV Fluids: Aggressive hydration is important because pancreatitis tends to lead to dehydration and shock.
- Pain Management: IV or oral painkillers (analgesics) to control severe pain.
- Nutritional Support: Patients are usually kept NPO (no food by mouth) initially to rest the pancreas. Nutrition is provided, either by a liquid diet or via a feeding tube (enteral nutrition). In very severe cases, IV nutrition (parenteral) may be needed.
- Treating the Underlying Cause: If gallstones are the culprit, an ERCP (endoscopic retrograde cholangiopancreatography) procedure is often done to remove the stone(s) blocking the duct.
Patients with gallstone pancreatitis should have their gallbladder removed (cholecystectomy) once stable to prevent recurrence. For alcohol-related cases, cessation of drinking is critical.
- Additional Care: In complicated cases (e.g. infected necrosis, abscess, or large pseudocyst), targeted interventions may be needed. These can include antibiotics for infection, drainage of fluid collections, or surgical debridement of dead tissue.
Intensive care support is used if organ failure (e.g. kidney or lung failure) occurs.
Treatment for Chronic Pancreatitis
- Lifestyle Changes: Complete abstinence from alcohol and smoking is essential; these worsen pancreatic damage. A low-fat diet can ease digestive workload.
- Pain Control: Long-term pain can be challenging. Treatment may involve pancreatic enzyme supplements (to aid digestion and reduce pancreatic stimulation), diabetes management (insulin for endocrine insufficiency), and various pain medications.
In some cases, procedures like nerve blocks (celiac plexus block) or surgery to remove painful scarred tissue are considered.
- Pancreatic Enzyme Replacement: Eventually, exocrine insufficiency develops in a number of patients. Pancreatic enzyme pills taken with meals help digest fats and nutrients. Vitamin supplements (A, D, E, K) may also be needed if malabsorption is severe.
- Monitoring and Surgery: Close follow-up is done in relation to complications (pseudocysts, diabetes).
In cases of unbearable pain localised to one part of the gland, surgical options include removing that part of the pancreas or even a total pancreatectomy if the damage is extensive. If diabetes develops, insulin therapy is initiated.
The majority of acute pancreatitis cases, which are mild, recover within one week. Chronic pancreatitis is a life-long condition; however, through the use of modern therapies, many patients are able to control their symptoms and continue living a quality life.
FAQs About Pancreatitis
- How is acute pancreatitis different from chronic pancreatitis?
Acute pancreatitis typically begins unexpectedly and is often resolved with treatment. Chronic pancreatitis is irreversible in the long run and cannot be overcome, resulting in continued pain and digestive problems. - What complications can pancreatitis cause?
Pseudocysts, necrosis or organ failure may develop in acute cases. Chronic pancreatitis can lead to malnutrition, diabetes, or risk of pancreatic cancer. - When should I seek medical help?
Call your physician as soon as possible in case of severe abdominal pain, particularly in instances when it spreads to your back or is accompanied by nausea, vomiting, fever, or jaundice.
- What diet is best for pancreatitis?
Begin with clear liquids and a low-fat diet, as recommended by your doctor. Consume low-fat, small meals that include fruits, vegetables, and protein. In chronic cases, enzyme supplements can be beneficial. - Is pancreatitis life-threatening?
Mild acute pancreatitis tends to go away, although severe ones can be deadly. Chronic pancreatitis is not typically life-threatening but may cause severe complications in the long run.
Conclusion
Pancreatitis can be challenging to manage, but being aware of its causes, symptoms, and treatment options can be the first step toward a successful management approach.
NEET PG aspirants can access a well-organised guide, clinically oriented learning, and high-yield information at DocTutorials to consolidate their understanding of key concepts. Join DocTutorials and explore our NEET PG course today!
Latest Blogs
-

NEET SS Exam 2024: Analysis, Key Dates, Counselling
The NEET SS 2024 exam kicked off on March 29, 2025. Over two days and two slots, candidates across 13…
-
NEET PG Registration 2025: An Essential Guide For Exam Prep
The NEET PG registration, which is conducted online, is a crucial step in the exam process. Filling out the NEET…
-
NEET PG Syllabus 2026: A Must-Have Complete Guide for Exam Success
The NEET PG Syllabus acts as one of the foundation stones for aspiring postgraduate medical students like you who are…




