Gaucher Disease | Causes, Symptoms, Diagnosis, and Treatment
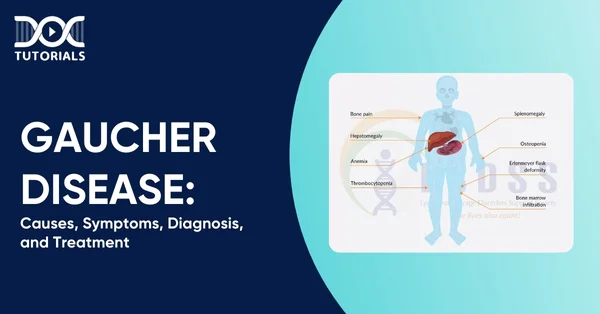
Gaucher disease (pronounced “go-SHAY”) is a chronic, rare inherited metabolic disorder where fatty materials, or lipids, accumulate in organs like the spleen, liver, and bone marrow. This condition is more common in people of Ashkenazi Jewish descent, with a prevalence of about 1 in 40,000 births to 1 in 100,000 births.
Understanding the causes, symptoms, diagnosis, and management of Gaucher disease is essential in improving patient outcomes. For medical students and healthcare professionals, particularly NEET PG aspirants, mastering such rare but high-yield biochemistry topics is vital for both academic excellence and effective clinical practice.
Keep reading for detailed insight!
Understanding Gaucher Disease and its Types
Individuals with Gaucher disease have a deficiency of the enzyme glucocerebrosidase, which is responsible for breaking down fatty substances called lipids. Instead, the lipids are deposited in specific organs, such as the spleen and liver, causing a variety of symptoms. This accumulation can cause the spleen and liver to enlarge significantly, impairing their normal function. The disease can also affect the lungs, brain, eyes, and bones.
Gaucher disease can be categorised into three types:
- Type 1
It is the most prevalent type, occurring in approximately 90% of the patients. Individuals with type 1 Gaucher disease experience low platelets in their blood that may result in excessive bruising and prolonged fatigue. Symptoms may appear at any age and may be an enlarged spleen or liver, kidney, lung, or bone issue.
- Type 2
This is the acute type that appears in infants, most often 3 to 6 months old, and usually the child will die. A majority of children with type 2 Gaucher disease do not live more than two years.
- Type 3
Type 3 involves skeletal issues, eye movement disorders, progressively worsening seizures, blood disorders, breathing difficulties, and enlargement of the liver and spleen.
What are the Symptoms of Gaucher Disease?
Although some of the symptoms have a general occurrence in all forms of Gauchers disease, each form of the disease possesses differentiating characteristics. The following is a detailed overview:
- Type 1
The signs are of varying intensities, and doctors can sometimes identify disease manifestations before the onset of symptoms. They often appear during childhood or adolescence but can occur at any age. Some common type 1 Gaucher disease symptoms are:
- Enlarged Organs
The spleen is usually significantly enlarged, and even the liver swells. This will result in:
- Easy bruising or bleeding because of blood platelets being trapped in the spleen.
- Damage in the spleen or liver or spleen scarring.
- Presence of pain or discomfort in the abdomen.
- Bone Conditions
Abnormal and brittle bones can result in:
- Pain in bones.
- Bone fractures even on slight injury.
- Bone Marrow Disorders
The bone marrow can fail to produce healthy blood cells in proper amounts, causing:
- Decreased blood platelet production, which results in bruising or easy bleeding.
- Decreased red blood cell production, causing weakness.
- Disease of the Lungs
Although the symptom is seen less often, the disease impacts breathing through:
- Damage to lung tissue.
- Restriction of the lungs due to swelling of the liver or spleen.
- Pulmonary hypertension.
- Growth Disorders
Some children with type 1 Gaucher disease will develop:
- Restricted or retarded growth.
- Delayed puberty.
- Type 2
Type 2 Gaucher disease is the rarest form. It causes rapid degeneration of cells in the brain stem, the part of the brain that controls vital functions like breathing and muscle control. Symptoms typically appear within the first few months of life, and death usually occurs within two years.
- Type 3
Type 3 Gaucher disease presents with symptoms similar to type 1, along with certain nervous system disorders and a progressive loss of brain cells. Symptoms usually begin during childhood and include:
- Eye movement disorders.
- Muscle spasms.
- Seizures.
- Loss of muscle control in adolescence or early adulthood.
- Dementia in adolescence or early adulthood.
What Causes Gaucher Disease?
Gaucher disease is an inherited metabolic disorder due to a mutation of the GBA gene. It is responsible for the production of an enzyme known as glucocerebrosidase (GCase), which performs various functions, among them being the breakdown of fats (sphingolipids) in the body.
People with Gaucher disease lack sufficient amounts of the enzyme. When the body doesn’t have enough GCase, fatty substances known as Gaucher cells build up in organs, bone marrow, and the brain. Excess fat causes various issues and symptoms, including the malfunction of organs, death of blood cells, and weakening of bones.
How is Gaucher Disease Diagnosed?
Gaucher disease diagnosis begins with the healthcare team evaluating the patient’s general health and medical history, including a physical examination. Diagnosis also takes into account:
- The description of the patient’s symptoms.
- Disease in family history.
- Blood test results.
Since Gaucher’s disease can occur with so many various symptoms, it is not always easy to diagnose.
What is the Treatment for Gaucher Disease?
Treatment for this condition varies with the patient’s age and type of Gaucher disease. No treatment is required in patients with mild symptoms.
Enzyme Replacement Therapy (ERT) is the treatment of choice for those with type 1 and for certain people with type 3 Gaucher disease. ERT relieves anaemia, improves bone density to prevent pain and fracture, and induces a decrease in the size of an enlarged spleen or liver.
Type 3 disease with brain or nervous system complications, including seizures, is less ideally treated by ERT because the drug is not able to pass the blood-brain barrier.
Standard ERT drugs are:
- Taliglucerase alfa (Elelyso)
- Imiglucerase (Cerezyme)
- Velaglucerase alfa (VPRIV)
These medications are administered intravenously (IV) and are typically given every two weeks in a session lasting 1 to 2 hours at a doctor’s office.
Alternative Treatments for Gaucher Disease
Other drugs for type 1 Gaucher disease are eliglustat (Cerdelga) and miglustat (Zavesca), which are tablets that are swallowed. These medications work by blocking the body’s process that causes fat buildup when there is an enzyme deficiency:
- Eliglustat
Eliglustat is a recently introduced medication that is consumed twice a day, but it won’t work for anyone whose body metabolises the drug too rapidly.
- Miglustat
Miglustat is intended for adults with mild to moderate type 1 Gaucher disease who have not responded to ERT and consume it in capsule form three times a day.
At present, no treatment exists to prevent the brain damage of type 3 Gaucher disease, although work continues to develop new therapeutic interventions.
Other therapies to manage symptoms are:
- Blood transfusions for anaemia.
- Medications to strengthen bones, prevent fat buildup, and ease pain.
- Joint replacement surgery to improve mobility.
- Surgery to remove a swollen spleen.
- Stem cell transplant to reverse type 1 symptoms. This procedure is complex and carries significant short-term and long-term risks, making it a rare choice.
- Pain management may involve acetaminophen or ibuprofen for mild pain or opioids for severe pain. Antidepressants, anti-anxiety drugs, and muscle relaxants may also help with pain.
- Vitamin D, calcium, or other supplements may alleviate Gaucher’s symptoms if dietary intake is insufficient.
Since the impact of Gaucher disease can differ across individuals, there must be close cooperation with a physician to provide proper care. Timely treatment can enhance the quality of life and, hopefully, increase the lifespan.
You can also participate in clinical trials, as scientists test new treatments for Gaucher disease using clinical trials. They determine the safety and effectiveness of new medicines, which can usually provide patients access to new drugs not yet available to the public. A physician can prescribe if a clinical trial might be a good choice.
FAQs About Gaucher Disease
- Can Gaucher disease be prevented?
Gaucher disease cannot be prevented when one has a genetic mutation. Genetic testing is advised for those at risk. Early treatment of type 1 Gaucher disease can prevent bone and organ damage.
- Is Gaucher disease dominant or recessive?
Gaucher disease is inherited autosomal recessively. That is, a person must have two copies of the gene in each cell, one from each parent, to be affected. Usually, both parents of a child who has an autosomal recessive condition will carry one copy of the abnormal gene but will not be affected themselves.
- Which organ is affected by Gaucher disease?
The spleen, liver, and bones are the organs most frequently affected by Gaucher disease. Type 1 occurs in more than 90% of all cases.
- Is Gaucher disease progressive?
Type 2 Gaucher disease (GD) is defined by primary central nervous system presentation with onset prior to the age of two years. It results in restricted psychomotor development and a rapidly progressive course, with death usually occurring within two to four years of age.
- Does Gaucher disease affect the heart?
Gaucher disease (GD) may seriously affect the heart. Calcific degenerative valve disease may have the potential to cause stenosis (narrowing) and regurgitation (leakage) of the heart valves. Aortic hypoplasia (underdevelopment of the aorta) is another established manifestation of GD.
Conclusion
A diagnosis of Gaucher disease can be overwhelming, bringing valid concerns about long-term health, future planning, or a child’s well-being. However, ongoing advancements in medical treatments and research offer significant hope. Most individuals can successfully treat symptoms and avert serious complications with proper individualised treatment and follow-up review.
For NEET PG candidates, a proper grasp of metabolic and genetic diseases, such as Gaucher disease, is essential not only to complete the biochemistry syllabus but also to acquire the requisite diagnostic skills required in clinical practice.
Platforms like DocTutorials can assist your preparation journey with concise video lectures, quick revision programmes (QRPs), and organised, high-yielding notes for academic as well as clinical preparedness. Start your NEET PG preparation with DocTutorials today!
Latest Blogs
-
-

NEET SS Exam 2024: Analysis, Key Dates, Counselling
The NEET SS 2024 exam kicked off on March 29, 2025. Over two days and two slots, candidates across 13…
-
NEET PG Registration 2025: An Essential Guide For Exam Prep
The NEET PG registration, which is conducted online, is a crucial step in the exam process. Filling out the NEET…