Erythema Nodosum: Causes, Symptoms, Diagnosis, and Treatment
Erythema Nodosum: Causes, Symptoms, Diagnosis, and Treatment
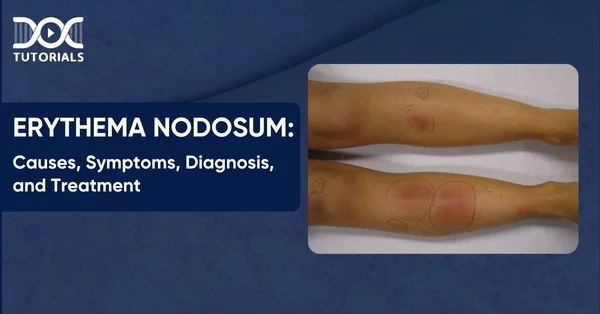
Erythema nodosum (EN) is a painful rash that appears like red or purple lumps on the front of the shins. It’s not only a skin problem; it can also be a sign of an infection, disease, or reaction to treatment.
EN is a kind of panniculitis, which means it affects the fat layer under the skin. It may be painful, and it could be an early symptom of more serious health problems that should not be disregarded.
This article helps you understand how skin symptoms progress and develop into systemic diseases. This topic is essential, especially for medical students preparing for the NEET PG exam. Keep reading to learn more about the causes, symptoms, diagnosis, and treatments of EN.
What is Erythema Nodosum?
Erythema nodosum (EN) develops when the fat layer under the skin gets inflamed. It causes painful, red or purple lumps, usually on the front of the shins. These lumps can feel warm and painful and can also appear on the thighs, forearms, chest, stomach, or back.
This is not an illness in itself; it is a reaction to an underlying health condition. It often shows up with diseases like COVID-19 or strep throat. Sulfa medications and penicillin are also known to cause such problems. Sometimes, EN is associated with long-term illnesses like Behçet’s disease or inflammatory bowel disease (IBD).
What are the Causes of Erythema Nodosum?
Infections, medicines, and other health problems are some of the recognised causes. Some of the other common erythema nodosum causes are:
- Infections
- Infections caused by streptococci, like strep throat
- Viral infections of the upper respiratory system, like colds and COVID-19
- Tuberculosis (TB)
- Hepatitis B and C
- Valley fever, also known as coccidioidomycosis
- Histoplasmosis is a fungal infection that comes from bird or bat droppings.
- Gastroenteritis caused by bacteria
- Chlamydia, gonorrhoea, and chancroid are all sexually transmitted infections.
- Medications
- Penicillin, amoxicillin, and ciprofloxacin are examples of antibiotics.
- Sulfa medicines include sulfamethoxazole and trimethoprim (Bactrim, Septra)
- Pills for birth control that you take by mouth
- Underlying Medical Conditions
- Crohn’s disease and ulcerative colitis are both types of inflammatory bowel disease.
- Sarcoidosis
- Fever from rheumatism
- Behcet’s illness
- Syndrome of Sweet
- Pregnancy
- Some malignancies, such as leukaemia and lymphoma
In many cases, EN is an indication of something more serious.
What are the Risk Factors of Erythema Nodosum?
Anyone of any age or background can get affected by EN, but certain factors increase the likelihood. Knowing these things helps with early detection and treatment. Here are some of the common risk factors of EN:
- Age: EN is most common in people between the ages of 20 and 40.
- Gender: Women are more impacted than men, perhaps because of hormones.
- Location: Individuals residing in areas where TB or certain fungal infections are more prevalent may be at a higher risk of contracting the disease.
- Medical Conditions: People with autoimmune illnesses or chronic infections or who take specific drugs are more likely to get EN.
What are the Symptoms of Erythema Nodosum?
Tender, red lumps that form under the skin, generally on the front of the shins, are the first symptoms of erythema nodosum (EN). These bumps feel like bruises and are warm to the touch. Over time, they develop into flat, purple, or brown areas that persist for weeks.
Some common signs are:
- Painful, red or purple bumps (nodules) under the skin
- Warmth and tenderness over the bumps
- A bruise-like appearance that disappears over weeks
- A low-grade fever
- Not feeling well (malaise)
- Tiredness
- Pain in the joints, especially the knees and ankles
- Lymph nodes that are swollen
- Cough
- Losing weight
- Pain in the stomach, throwing up, or diarrhoea
EN mostly affects the front of the lower legs; however, it can also show up on the thighs and other areas, like:
- Calves
- Buttocks
- Ankles
Identifying these signs early will make it easier to determine the cause and receive the appropriate therapy.
What is the Diagnosis of Erythema Nodosum?
The first step in diagnosing erythema nodosum (EN) is to review an extensive medical history and conduct a thorough physical examination. Doctors perform various tests to determine the cause of EN.
Some common steps in diagnosis are:
- Physical Exam: The doctor will look at the affected skin and ask about any other symptoms and the medical history.
- Blood Tests: These may include,
- Erythrocyte sedimentation rate (ESR)
- Complete blood count (CBC) with differential
- Level of C-reactive protein (CRP)
- Culture tests: They include,
- Strep throat culture is used to look for infections
- Stool culture to look for parasites or IBD
- Chest X-ray: This helps look for lung infections or sarcoidosis that could be linked to EN.
- Skin Biopsy: This is when a small piece of skin is examined under a microscope. If the diagnosis remains unclear after the mentioned tests, a skin biopsy is done.
These not only help diagnose EN, but they also aid in planning treatment by identifying infections or other conditions associated with it.
What are the Treatment Options for Erythema Nodosum?
The treatment for erythema nodosum (EN) depends on the underlying cause and the severity of the symptoms. In many cases, EN typically resolves on its own within a few weeks to a few months. However, if the symptoms persist or become too painful, the focus of treatment shifts to reducing inflammation and identifying the underlying cause.
Common erythema nodosum treatment options include:
- Treating the Underlying Condition: Manage infections, inflammatory diseases or other conditions that caused EN.
- Stopping the Consumption of the Triggering Medication – If a medication caused EN, the doctor may advise the patient to stop it. Always consult a doctor before stopping any medication.
- Symptom Relief through Medication:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen to reduce pain and swelling
- Corticosteroids for more severe cases
- Potassium iodide solution to reduce inflammation in some patients
- Analgesics for pain management
- Lifestyle Support:
- Elevate the affected limb to reduce swelling
- Get plenty of rest and avoid strenuous activity
With proper care and treatment of the cause, most people recover fully without any long-term effects.
How to Prevent Erythema Nodosum?
The prevention of erythema nodosum (EN) is not always possible, but the likelihood of it occurring or worsening can be reduced, especially if the triggers that cause it are well-managed.
Here are some useful tips for lowering the risk of erythema nodosum:
- Avoid medications that can make the condition of the EN worse. If the patient has had EN before, they must avoid penicillin, sulfa pills, or certain antibiotics, but only if the doctor recommends.
- Address any underlying health issues. Keeping illnesses like inflammatory bowel disease or sarcoidosis under control may lower the likelihood of EN recurrence.
- Limit the exposure to illnesses by avoiding contact with people who are sick with viral or bacterial diseases, especially strep throat or respiratory infections.
- Get vaccinated on time. Immunisation can stop diseases that are connected to EN.
- Keep your hands clean and follow proper hygiene habits to minimise the risk of getting sick.
- Maintain a healthy immune system. A balanced diet that doesn’t trigger inflammation, regular exercise, and a healthy weight can help keep your body strong.
Not all causes can be identified or avoided, but these steps can significantly reduce the likelihood of EN episodes.
FAQs About Erythema Nodosum
1. Is erythema nodosum life-threatening?
No, erythema nodosum itself is not fatal. The bumps and other issues will typically resolve within a few weeks to a few months. But if EN is a sign of a major underlying ailment, that condition can be deadly.
2. What foods should you avoid if you have erythema nodosum?
There is no special diet recommended for individuals with erythema nodosum. But it’s always a good habit to eat well. Researchers are still investigating how certain meals can exacerbate inflammation and symptoms.
3. What is the first thing that should be done to treat erythema nodosum?
The first step in treatment is to ease symptoms. This includes putting the injured limb up, using compression bandages, and using NSAIDs such as indomethacin (100–150 mg/day) or naproxen (500 mg/day) to ease discomfort and swelling.
4. What is the best way to treat erythema?
If the symptoms of erythema are minimal, you don’t need to treat them. Depending on where the symptoms are, topical corticosteroids, oral antihistamines, or ocular drops may be employed.
5. What kinds of blood tests are done for erythema nodosum?
A complete blood count with differential, C-reactive protein, a throat swab, and ASO titres are all important assays. You may also receive a chest X-ray to screen for diseases such as tuberculosis or sarcoidosis.
Conclusion
Erythema nodosum (EN) is more than a skin condition—it’s an underlying infection, autoimmune issue, or medication side effect. It is essential to recognise the symptoms early—painful red lumps on the shins and understand the causes to diagnose and treat them on time.
If you are a medical student or preparing for NEET PG, understanding conditions like EN is a part of your clinical foundation. At DocTutorials, you will find a complete library of medical topics along with high-quality video lectures, test series, expert insights, and detailed question banks to help you prepare well.
Explore our NEET PG course and elevate your preparation to the next level.
Latest Blogs
-

NEET PG Exam 2025- Date, Pattern, Marking Scheme, Subject Wise Weightage, and Exam Mode
NEET PG Exam 2025 is the ultimate gateway for medical graduates aspiring to pursue postgraduate courses in medicine, including MD,…
-

INI CET Exam 2025: Your Roadmap to Success – Key Topics, Strategies, and Lessons from Last Year’s Papers
The INI CET exam is more than just a test; it’s a significant milestone for many medical students aiming to…
-

INI CET Exam Success: Previous Year Question Papers & Ultimate Guide – INI CET PYQ
One can feel overwhelmed while preparing for the INI CET (Institute of National Importance Combined Entrance Test). A vast syllabus,…




