Giardiasis: Causes, Symptoms, Diagnosis, and Treatment
Giardiasis is caused by Giardia lamblia, also known as G. intestinalis or G. duodenalis. It was first observed by A. V. Leeuwenhoek in 1681 while examining his stool. Later, it was described and named after Dr F Lambl and Professor A Giard (1859).
G. lamblia has a worldwide distribution and is considered one of the most common parasites, causing both endemic and epidemic intestinal diseases and diarrhoea. Grasping the causes, symptoms, diagnosis, and treatment strategies for giardiasis is valuable not only for patient care but also for NEET PG aspirants.
Read on for an in-depth exploration of giardiasis and its implications in the field of medicine.
What is Giardiasis?
Giardiasis is an intestinal infection caused by the protozoan parasite Giardia lamblia. The parasite inhabits the small intestine and is transmitted via the faeco-oral route. The prevalence in children ranges from 0.5% to 70%.
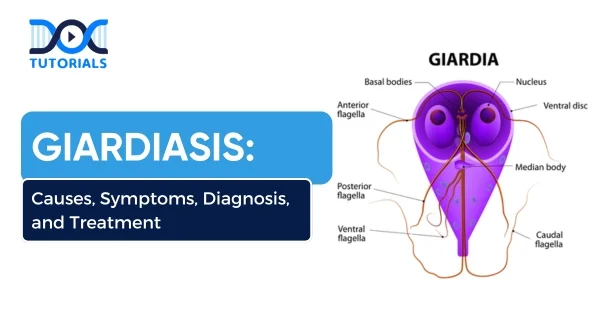
Giardia inhabits the crypts of the duodenum and the upper part of the jejunum in man. It occurs in two forms:
1. Pear-shaped Trophozoite: It is the pathogenic form and feeding stage of the parasite.
2. Tetra-nucleated Oval Cyst: It is the infective form as well as the diagnostic form of the parasite.
What are the Causes and Risk Factors of Giardiasis?
The primary route of infection is ingesting cysts of Giardia lamblia, usually through contaminated:
- Drinking water (especially untreated or from lakes and streams)
- Food washed with contaminated water
- Hands or surfaces (especially in childcare settings)
Trophozoites are the pathogenic form; they adhere to the duodenal mucosa, disrupting the intestinal epithelium, which leads to increased permeability and malabsorption. Trophozoites do not invade the mucosa but feed on mucus secretions.
Malabsorption:
- Malabsorption of Fat (steatorrhea): This leads to foul-smelling, profuse, frothy diarrhoea
- Disaccharidase Deficiencies (lactose, xylose): Leading to lactose intolerance
- Malabsorption of vitamin A, B12 and iron
- Protein-losing enteropathy
Antigenic Variation:
Due to a cysteine-rich protein on its surface, known as the variant surface protein (VSP), giardia undergoes frequent antigenic variations. This helps the parasite evade the host’s immune system, leading to the persistence of the infection and resulting in chronic and recurrent illness.
Risk Factors:
- Travellers to regions with inadequate sanitation.
- Campers and hikers who drink untreated water.
- Children in daycare centres.
- Immunocompromised individuals (however, it does not appear to be associated with HIV/ AIDS).
- Men who have sex with men (MSM) are at increased risk due to increased oral-faecal exposure.
What are the Symptoms of Giardiasis?
Symptoms typically begin 1–2 weeks after exposure and may persist for 2–6 weeks or longer. Common giardiasis symptoms include:
- Asymptomatic Carriers:
Most infected individuals are asymptomatic, harbour the cysts in the gut, and spread the infection.
- Acute Giardiasis:
The incubation period varies from 1 week to 3 weeks, and common symptoms include:
- Diarrhoea, abdominal pain, bloating, belching, flatus, and vomiting.
- Fatty Diarrhoea (steatorrhea): Diarrhoea is often foul-smelling with fat, cellular exudate, and mucus but no blood.
- Giardia is an essential cause of traveller’s diarrhoea.
3. Chronic Giardiasis:
It may present with or without a previous acute symptomatic episode. Here is an overview of its signs:
- GI Symptoms: Include recurrent episodes of foul-smelling diarrhoea, foul flatus, sulfurous belching with rotten egg taste, and profound weight loss leading to growth retardation.
- Extraintestinal Manifestations: Have been reported, including urticaria, arthritis, anterior uveitis, and retinal changes resembling salt-and-pepper patterns.
What is the Diagnosis Process for Giardiasis?
The diagnostic methods of giardiasis are as follows:
- Stool Examination
Stool microscopy is considered the gold standard for diagnosing giardiasis, which detects both cysts and trophozoites:
- Trophozoites adhere firmly to the duodenal mucosa by an adhesive disc, leading to intermittent shedding. Hence, repeated stool examination (at least three samples collected on alternate days within 10 days) should be done.
- Pus cells or blood (RBCs) will never be seen in stool microscopy in the case of giardiasis. If found, it suggests an alternative diagnosis.
- Sensitivity ranges from 60% to 80% with a single stool and increases to more than 90% after three stool examinations.
- Concentration techniques, such as zinc sulphate flotation or formalin ether sedimentation methods, are employed to increase the chance of detection.
- Duodenal Sampling: In case the stool examination result is negative, then direct duodenal samples, such as aspirates (obtained by entero-test) or biopsies (performed by endoscopy), should be processed.
- Permanent stains, such as trichrome stains, can be used to demonstrate cysts and trophozoites in stool.
- Entero-test (or String Test)
This process involves using a gelatin capsule attached to a thread containing a weight. Here is a detailed overview:
- One end of the thread is attached to the outer part of the patient’s cheek, and then the capsule is swallowed.
- The capsule dissolves in the stomach, releasing threonine, which is then carried to the duodenum, where it is absorbed and taken up by the duodenal cells.
- Four hours later, the thread is withdrawn and shaken in saline to release trophozoites, which can be detected microscopically by either a wet mount or a permanent stained smear.
- The entero-test is also helpful in detecting other upper intestinal parasites, such as strongyloides, cryptosporidium, and clonorchis.
- Histopathology
Endoscopy-guided duodenal biopsy tissue can be processed by touch preparation and stained with Giemsa stain to demonstrate the trophozoites.
- Antigen Detection in Stool
Enzyme-linked Immunosorbent Assay (ELISA) and direct fluorescent antibody tests are available using labelled monoclonal antibodies against cyst wall protein antigens. Both tests are highly sensitive and specific. They are instrumental in the microscopy of negative samples and also in outbreak situations.
Rapid ICT has been developed that simultaneously detects antigens of giardia (alpha-1 giardin antigen), Entamoeba histolytica and cryptosporidium with comparable sensitivity and specificity to ELISA.
- Antibody Detection
Both ELISA and indirect fluorescent antibody (IFA) formats are developed to detect antibodies in the serum:
- However, unlike microscopy and antigen detection, the presence of antibodies cannot distinguish between recent and past infections.
- Hence, serology is only helpful for epidemiological purposes for estimating the prevalence of infection.
- Culture
Giardia can be cultivated in axenic media, such as Diamond’s medium, used for E. histolytica. Culture is done for research purposes and to prepare the antigens.
- Molecular Methods
Detection of giardia nucleic acid in stool and environmental samples (such as water) by polymerase chain reaction (PCR) or gene probes is highly sensitive and specific. PCR can detect as low as 1–2 cysts in the sample.
- BioFire FilmArray: It is a fully automated commercial PCR system from bioMérieux. The gastrointestinal panel is used to detect common bacterial, viral, and parasitic pathogens (cryptosporidium, cyclospora, E. histolytica, and giardia) that cause diarrhoeal diseases.
- Molecular Typing: Can detect genotypes and assemblages by sequencing several genes, such as glutamate dehydrogenase (gdh) and β-giardin (bg).
- Radiological Finding
- Fluoroscopy may reveal hypermotility at the duodenal and jejunal levels.
- X-ray after a barium meal may reveal nonspecific irregular mucosal thickening with large, dilated loops of hypotonic bowel (positive in 20% of cases). A barium meal may interfere with the stool examination. So, stool samples should be collected before the barium meal.
What are the Treatment Options for Giardiasis?
Most patients respond well to antiparasitic medications. Common giardiasis treatments include:
| Drug Name | Typical Dose & Duration | Notes |
| Metronidazole | 250–500 mg TID x 5–7 days | Most commonly used |
| Tinidazole | A single dose of 2 g orally | Effective alternative |
| Nitazoxanide | 500 mg BID x 3 days | Well-tolerated in children & adults |
| Albendazole | 400 mg daily x 5 days | Less used; some resistance noted |
Additional pointers to remember:
- Ensure hydration and electrolyte replacement for symptomatic cases.
- For resistant or relapsing infections, switching to a different drug or extending the course may be necessary.
- Treat asymptomatic carriers in high-risk settings (e.g., daycare centres) to prevent the spread.
What are the Prevention Strategies for Giardiasis?
Giardiasis can be prevented by:
- Improved food and personal hygiene
- Boiling or filtering of potentially contaminated water
- Treatment of asymptomatic carriers
No vaccine is currently available.
FAQs About Giardiasis
- Can giardiasis spread from person to person?
Yes. It spreads via the faecal-oral route. Close contact, poor hygiene, or contaminated hands and surfaces can transmit the infection.
- Is giardiasis contagious even when there are no symptoms?
Yes. Asymptomatic individuals can shed cysts in their stool and infect others.
- Can giardiasis be resolved without treatment?
Mild cases may clear on their own, but treatment shortens illness duration and prevents transmission.
- Are there any vaccines for giardiasis?
No vaccines are currently available. Prevention relies on maintaining hygiene, practicing safe food handling, and ensuring water treatment.
- Can pets give me giardiasis?
Possibly. Dogs and cats can carry giardia, but transmission to humans is rare with proper hygiene.
Conclusion
Giardiasis is a common yet preventable parasitic infection with a global impact. For medical aspirants, understanding the transmission, clinical features, and giardiasis treatments is critical for both exams and real-world scenarios. With timely diagnosis and appropriate care, outcomes are excellent.
Continue to review high-yield parasitology and infectious disease topics to stay ahead in your NEET PG prep journey. For structured guidance and targeted content, rely on DocTutorials to simplify complex concepts and focus on clinical relevance.Check out our NEET PG guide today!
Latest Blogs
-

NEET PG Exam 2025- Date, Pattern, Marking Scheme, Subject Wise Weightage, and Exam Mode
NEET PG Exam 2025 is the ultimate gateway for medical graduates aspiring to pursue postgraduate courses in medicine, including MD,…
-

INI CET Exam 2025: Your Roadmap to Success – Key Topics, Strategies, and Lessons from Last Year’s Papers
The INI CET exam is more than just a test; it’s a significant milestone for many medical students aiming to…
-

INI CET Exam Success: Previous Year Question Papers & Ultimate Guide – INI CET PYQ
One can feel overwhelmed while preparing for the INI CET (Institute of National Importance Combined Entrance Test). A vast syllabus,…




