Immune Thrombocytopenic Purpura: Causes, Symptoms, Diagnosis, and Treatment
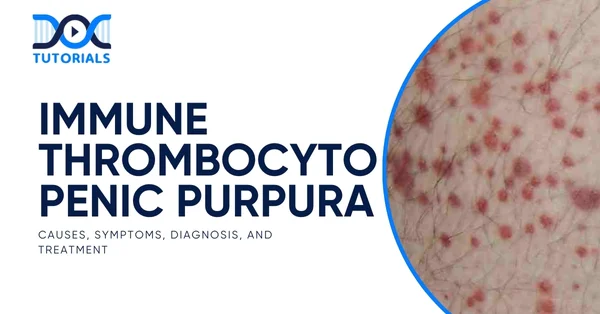
Immune thrombocytopenic purpura (ITP) is a haematological disorder marked by autoimmune destruction of platelets, leading to bleeding risks despite otherwise healthy appearance of the person. ITP can often pose a difficult diagnostic challenge in clinical presentation.
Its characteristic feature is the destruction of platelets without an evident secondary cause, and it is an archetype of immune-mediated thrombocytopenia. Understanding this condition is essential for medical students not only in terms of hematologic assessment and treatment protocols, but also for competitive exams such as the NEET PG.
Keep reading to know more about immune thrombocytopenic purpura.
What is Immune Thrombocytopenic Purpura?
Immune thrombocytopenic purpura or idiopathic thrombocytopenic purpura is an autoimmune disease in which the immune system of the body attacks platelets, which are small cells involved in blood coagulation. It is also associated with low platelet levels, and its symptoms include purpura, petechiae and bleeding of myoderms.
Pathophysiologically, platelets are covered with IgG (immunoglobulin A) autoantibodies that are destroyed more rapidly by splenic macrophages and, in some cases, produced less effectively in the bone marrow.
What are the Types of Immune Thrombocytopenic Purpura?
ITPs are mainly classified into 2 categories:
1. Acute Immune Thrombocytopenic Purpura
- It is a self-limiting disease
- Common in children aged 2-4 years
- Presents 1-3 weeks after viral (measles, rubella, EBV) infection
- Platelet destruction by antiplatelet autoantibodies
- The platelet count is decreased, sometimes even below 10,000/μL (10 × 10^9/L)
2. Chronic Immune Thrombocytopenic Purpura
- Persistent thrombocytopenia for more than 6 to 12 months
- Females are more affected than males (Female: Male = 3:1)
- More common and usually seen in adults (20 to 40 years)
What Causes Immune Thrombocytopenic Purpura?
It is an autoimmune disorder (type II hypersensitivity reaction) characterised by the development of antiplatelet antibodies. The antibodies (most commonly IgG type) attach to the platelet antigens (usually lb-Illa or lb-IX of platelets).
Approximately 80% of patients have antiplatelet antibodies, which typically represent antiplatelet IgG. Opsonin C3b (complement component 3b) is formulated by activation of the complement.
Antibody- and complement-mediated opsonisation of platelets results in phagocytosis of platelets by RE (reticuloendothelial) system phagocytes (primarily the spleen) through Fc (fragment crystallizable receptor) or C3b receptors.
This causes platelet destruction. In patients, splenectomy results in significant improvement in 75-80% of cases.
What are the Risk Factors of Immune Thrombocytopenic Purpura?
For immune thrombocytopenic purpura, it’s crucial to assess the presence of potential risk factors:
| Risk Factor | Description |
| Recent Viral Infections | It is common in children and contains viruses such as EBV (Epstein-Barr Virus), influenza, mumps, measles, and rubella. Triggers an immune response. |
| Autoimmune Disorders | Diseases like SLE (Systemic Lupus Erythematosus) and rheumatoid arthritis also raise the risk as they are associated with an autoimmune disease. |
| Helicobacter pylori Infection | ITP in adults may be related to chronic H. pylori; eradication therapy can lead to an increase in platelet count. |
| Medications | Antiepileptics like quinine, heparin, and other medications can lead to thrombocytopenia or imitate ITP. |
| Gender and Age | Found more often in females aged 30 to 50 years old. In children, there is an acute, self-limiting form of presentation. |
What are the Symptoms of Immune Thrombocytopenic Purpura?
Recognising immune thrombocytopenic purpura symptoms early is essential for timely management. Patients may be entirely asymptomatic or exhibit:
- Petechiae (tiny red flat spots), purpura, and easy bruising
- Mucosal bleeding, nosebleeds, gum bleeding, menorrhagia
- In severe cases, life‑threatening haemorrhage (e.g., intracranial bleeding)
- Sudden onset
- Epistaxis and mild fever
What is the Diagnosis of Immune Thrombocytopenic Purpura?
The standard approach to diagnosis includes:
- Peripheral Blood Count
- Platelet Count: Markedly reduced below 80,000/cu mm (80×109/L).
- Haemoglobin: Ranges from 7-12 g/dL.
- Peripheral Smear
- Platelets: Markedly reduced (thrombocytopenia) and abnormally large-sized platelets (megathrombocytes/giant platelets)
- Red Blood Cells (RBCs): Chronic blood loss (e.g., menorrhagia) due to ITP may lead to microcytic hypochromic anaemia
- White Blood Cells (WBCs): Normal
- Bone Marrow Examination
- Cellularity: Hypercellular
- Megakaryopoiesis:
- Moderate increase in the number of both immature and mature forms of megakaryocytes
- Immature megakaryocytes predominate, characterised by large, nonlobulated single nuclei and basophilic cytoplasm
- Erythropoiesis:
- Prolonged bleeding may cause anaemia, leading to normoblastic erythroid hyperplasia
- Constant bleeding leads to iron deficiency and micronormoblastic erythroid hyperplasia
- Myelopoiesis: Normal
- Storage Iron: Severe and chronic bleeding can cause iron deficiency, leading to depleted iron stores
- Bleeding Time (BT): Prolonged, but prothrombin time (PT) and partial thromboplastin time (PTT) are standard
- Tourniquet Test: Positive
- Clotting Time: Normal
- Tests for Platelet Autoantibodies: May be positive
What are the Treatment Options for Immune Thrombocytopenic Purpura?
The goal of immune thrombocytopenic purpura treatments is to prevent significant bleeding and improve quality of life. Treatment involves:
1. Observation
- Most children, and approximately 30% of adults, resolve spontaneously without intervention within several months to a few years
- Observation is recommended if platelet counts are >30 × 10⁹/L and bleeding is absent or minor
2. First‑Line Therapies
- Corticosteroids (oral prednisone or dexamethasone in high dose) are the usual first-line therapy to help inhibit the production of autoantibodies and limit platelet destruction.
- Intravenous immune globulin (IVIg) or anti-D immunoglobulin (for Rh-positive patients) can be used to achieve a rapid increase in platelet counts, which can be valuable in pre-procedure or acute bleeding settings.
3. Second‑Line Treatments
These are used when the first-line fails or a relapse occurs:
- Thrombopoietin Receptor Agonists (TPO-RAs): Include eltrombopag and romiplostim, which promote platelet production in chronic ITP.
- Rituximab: An off-label anti-CD 20 monoclonal antibody mainly in those adults with a refusal of splenectomy.
- Fostamatinib: Orally available drug that decreases platelet destruction via lack of the macrophage pathway.
4. Splenectomy
- It achieves durable remission in 60% to 80% of cases, but relapse rates vary
5. Other Immunosuppressives
- Agents such as dapsone, azathioprine, or mycophenolate may be used when other therapies are insufficient
FAQs About Immune Thrombocytopenic Purpura
- Can ITP resolve without treatment?
Yes, 70-80% of patients get better within six months, particularly children. In adults, approximately 30% may spontaneously recover within a year. - Are there long-term side effects of corticosteroids?
Yes, prolonged use of steroids does lead to osteoporosis, weight gain, diabetes, cataracts, and other metabolic effects; thus, they are reduced and tapered with caution. - When is splenectomy considered?
Splenectomy is an option in adults with chronic, refractory ITP that relapses or fails second-line treatment options, after surgery risk and bleeding risks are considered. - What’s the role of thrombopoietin receptor agonists?
TPO-RAs, such as romiplostim or eltrombopag, enhance the platelet count and are particularly useful in chronic refractory ITP.
Conclusion
In infants, the progression of ITP is usually acute and self-limiting, while in adults, active treatment is required. The diagnosis is based on the exclusion of other causes of thrombocytopenia and depends on the results of the diagnostic tests.
Medical aspirants should be equipped with knowledge of pathophysiology and evidence-based management to apply these concepts in real-world practice and crack the competitive exams.
Join DocTutorials today and explore our NEET PG course to excel in your medical career.
Latest Blogs
-
NEET PG Exam 2025- Date, Pattern, Marking Scheme, Subject Wise Weightage, and Exam Mode
NEET PG Exam 2025 is the ultimate gateway for medical graduates aspiring to pursue postgraduate courses in medicine, including MD,…
-

INI CET Exam 2025: Your Roadmap to Success – Key Topics, Strategies, and Lessons from Last Year’s Papers
The INI CET exam is more than just a test; it’s a significant milestone for many medical students aiming to…
-
INI CET Exam Success: Previous Year Question Papers & Ultimate Guide – INI CET PYQ
One can feel overwhelmed while preparing for the INI CET (Institute of National Importance Combined Entrance Test). A vast syllabus,…