Xerosis: Causes, Symptoms, Diagnosis, and Treatment
Xerosis, or excessively dry skin, is a prevalent complaint that affects individuals of every age, especially during cold weather months or as a result of pre-existing conditions. For the next generation of clinicians, knowing the causes, symptoms, and treatment modalities of xerosis is crucial.
Untreated, xerosis can lead to complications like skin cracking and secondary infections. Let’s walk through the major causes, clinical features, diagnosis, and xerosis treatment strategies—presented clearly for NEET PG aspirants and medical students.
Keep reading!
What is Xerosis?
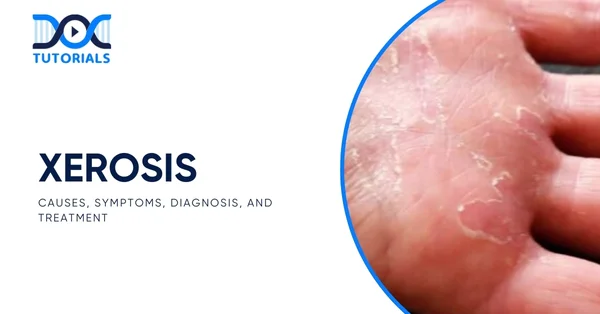
Xerosis, also known as xerosis cutis or xeroderma, is a medical condition characterised by abnormally dry, rough, and often itchy skin due to a lack of moisture and natural oils. It typically takes the form of flaky, scaly, or cracked skin patches and may be anywhere from mild dryness to extreme discomfort with bleeding or potential infection.
Xerosis can develop in anyone, but is especially prevalent in the elderly because the skin’s ability to hold water declines with age. The condition can be precipitated or exacerbated by environmental causes such as cold temperatures, repeated washing, irritating soaps, or medical conditions, including diabetes or hypothyroidism.
Though usually transient and treatable, untreated xerosis has the potential to cause complications such as skin cracks and secondary bacterial infections.
What are the Causes of Xerosis?
Dry skin happens when the skin loses excessive water or natural moisturising factors. A number of internal and external causes lead to this loss of moisture. The following are the major causes that predispose an individual to the development of xerosis:
- Exposure to Heat: Central heating, space heaters, wood stoves, and fireplaces lower indoor humidity and make the skin dry.
- Cold or Dry Climates: Residing in windy, low-humidity, or cold weather results in increased water loss from the skin.
- Excessive Bathing or Scrubbing: Taking long, hot showers or scrubbing excessively strips the skin of its natural oils, causing dryness.
- Harsh Soaps and Cleansers: Most commercial soaps, shampoos, and household cleansers remove essential oils from the skin.
- Ageing: As people grow older, skin thins and decreased oil production makes it lose its ability to hold moisture.
- Dehydration and Poor Diet: Inadequate water consumption and nutritional deficiencies can impact the hydration of the skin.
- Genetics: Dry skin as a genetic trait, a family history of allergic skin conditions, and personal history of allergic skin conditions.
- Occupational Risks: Hands-on jobs that require frequent handwashing, or full-water immersion (i.e., healthcare workers, hairstylists, farmers, masons, etc.)
- Chlorinated Water: Regular exposure to chlorinated swimming pool water can deplete oils from the skin.
- Other Health Conditions: Conditions including hypophosphatemia, diabetes, hypothyroidism, malnutrition, and chronic disease of the kidneys all increase the risk of developing xerosis.
What are the Symptoms of Xerosis?
Common symptoms of xerosis cutis are as follows:
- Skin that appears dry, itchy, and scaly, particularly on the arms and legs
- Skin that feels taut, especially following a bath
- White, flaky patches on the skin
- Red or pink irritated areas
- Mild to severe scaling or peeling
- Itchiness (pruritus)
- Fine lines or fissures
- Mild to severe flaking skin, leading to an ashy appearance that can affect dry, brown and black skin
- Cracked appearance resembling a “dry riverbed” on the legs
- Skin that varies from reddish on lighter skin to greyish on darker skin
- Deep fissures that may result in bleeding
How to Diagnose Xerosis?
A medical professional will generally look at the areas that are affected as well as gather a little bit of history about your symptoms, skin care, bathing behaviour, and history of other medical problems.
The medical provider will usually examine environmental and lifestyle factors. If the dryness is chronic or serious, tests could be suggested to rule out problems such as hypothyroidism, psoriasis, or dermatitis, which have similar symptoms.
What is the Treatment for Xerosis?
Common approaches adopted in order to treat and manage xerosis include the following:
- Stay Away from Drying Ingredients: Look for skincare products that contain severe ingredients such as alcohol, added scents, etc., that affect the moisture of the skin.
- Apply Natural Moisturisers: Coconut oil, sunflower seed oil, oatmeal, and honey possess natural moisturising and anti-inflammatory properties that ease and guard dry skin.
- Moisturise Regularly and Well: Moisturise soon after bathing and use healing creams in the evening. Opt for products with glycerine, urea, or other humectants that ensure more skin hydration.
- Replace Harsh Cleansers: Use mild, fragrance-free cleansers with moisturising agents like propylene glycol or glycerine to avoid drying the skin further.
- Exfoliate Gently: Gently strip away dead skin flakes with a gentle towel or exfoliating cleanser, and always follow with a moisturiser to trap in moisture.
- Take Cooler, Briefer Showers: Keep showers to 5–10 minutes with warm water to protect the skin’s natural barrier against dryness.
- Eat a Healthy Diet: Add foods high in omega-3 fatty acids, vitamins C, D, E, K, and minerals zinc and copper to promote skin health from the inside out.
- Stay Hydrated: Drink lots of water during the day and eat foods that contain high water content, such as cucumbers and watermelon, to ensure internal hydration.
- Humidify Your Space: Employ a humidifier, particularly in arid environments or cold weather, to maintain skin moisture and avoid extreme dryness.
- Shield Skin from Extreme Weather: Use scarves, gloves, or protective wear on exposed areas in cold, dry weather to protect against environmental stress.
- Restrict Sun Exposure: Apply a broad-spectrum sunscreen with a minimum SPF 30 when outside, as UV (ultraviolet) radiation can dry out skin and exacerbate xerosis.
FAQs about Xerosis
- What is the most effective initial treatment for xerosis?
The most effective initial treatment for xerosis is usually handled with over-the-counter moisturising creams along with proper home care.
- What is the origin of the term xerosis?
Xerosis cutis refers to a medical condition characterised by excessively dry skin. The term is derived from the Greek word “xero,” which translates to dry.
- What major factors trigger xerosis?
Xerosis tends to occur more in people with comorbid medical conditions like type 2 diabetes, obesity (≥ 30 BMI), or chronic liver illnesses like cirrhosis, particularly in those with hepatitis B or C infections or alcohol abuse. Such conditions interfere with the skin’s capacity to hold water, thus resulting in enhanced dryness.
- What are the complications of dry skin?
If untreated, dry skin can result in complications such as atopic dermatitis (eczema), where the skin becomes inflamed, cracked, and itchy. Deep cracks can also form, further making the skin susceptible to bacterial infections as the protective function of the skin is lost.
- What should be the diet of a patient suffering from xerosis?
To help manage dry skin symptoms, patients should avoid foods and drinks that dehydrate the body, such as alcohol, caffeine, salt, and sugar. Instead, they need to consume nutrient-dense foods like fruits, vegetables, healthy fats, etc., and focus on drinking plenty of water.
Xerosis is more than dry skin—it’s a dermatologic disease that demands attention by clinicians. Knowledge of its pathogenesis, clinical presentation, and treatment ensures timely and appropriate management. With reinforcement of skin hydration and resolution of underlying reasons, xerosis is generally reversible with proper care.
Medical students preparing to sit for the NEET PG exam should be familiar with such skin conditions. To help them out, DocTutorials dissects complicated diseases into comprehensible, simple concepts—perfect for determined aspirants.
Join DocTutorials today and explore our NEET PG course to excel in your medical career.
Latest Blogs
-

NEET PG Exam 2025- Date, Pattern, Marking Scheme, Subject Wise Weightage, and Exam Mode
NEET PG Exam 2025 is the ultimate gateway for medical graduates aspiring to pursue postgraduate courses in medicine, including MD,…
-

INI CET Exam 2025: Your Roadmap to Success – Key Topics, Strategies, and Lessons from Last Year’s Papers
The INI CET exam is more than just a test; it’s a significant milestone for many medical students aiming to…
-

INI CET Exam Success: Previous Year Question Papers & Ultimate Guide – INI CET PYQ
One can feel overwhelmed while preparing for the INI CET (Institute of National Importance Combined Entrance Test). A vast syllabus,…




