Anthrax: Causes, Symptoms, Prevention, and Treatment
Anthrax is a rare but deadly bacterial infection caused by Bacillus anthracis, which is found in the soil. It affects both humans and animals and can be spread through inhalation, ingestion, or skin contact. Although rare, anthrax can be life-threatening if not treated on time.
Learning about anthrax is essential for medical aspirants and healthcare providers, as it provides an in-depth knowledge of infectious diseases, their transmission, and public health risks.
This guide breaks it down in simple terms—because awareness can save lives.
What is an Anthrax?
Anthrax (pronounced “AN-thraks”) is a serious infectious disease caused by exposure to Bacillus anthracis, a bacteria that is found in a dormant state in the soil. It affects grazing animals like cattle, sheep, and goats, but humans can get it through direct contact with infected animals or contaminated animal products.
Once inside the body, the spores become active, multiply rapidly, and release toxins that can cause severe illness or death if left untreated.
How Do People Get Anthrax – Key Causes
Bacillus anthracis, a bacteria that lives in the soil, forms spores that can sit dormant for years until they enter a host. Livestock like cattle, sheep, goats, and even wild animals like deer will inhale or ingest these spores while grazing.
Humans get infected through:
- Inhalation – Breathing in spores from animal products.
- Ingestion – Eating or drinking contaminated food or water.
- Skin contact – Spores entering through cuts or wounds.
Once inside the body, the spores activate, multiply, and release toxins, infecting the host.
What are the Signs and Symptoms of an Anthrax Infection?
Anthrax symptoms vary depending on how you get infected. In most cases, they show up within 6 days, but inhalation anthrax can take weeks to develop. There are four types of anthrax infections:
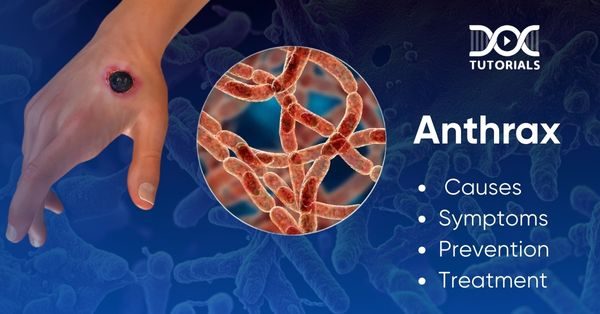
- Cutaneous Anthrax (Skin Infection)
The most common and mildest, cutaneous anthrax occurs when spores get in through cuts or sores. Symptoms include:
- A raised, itchy bump that turns into a painless sore with a black centre.
- Swelling around the sore and nearby lymph glands.
- Fever and headache in some cases.
- Gastrointestinal Anthrax (Ingested Infection)
Eating undercooked meat from an infected animal can give you anthrax in the digestive system. Symptoms include:
- Nausea, vomiting, and loss of appetite.
- Severe abdominal pain and bloody diarrhoea in advanced stages.
- Fever, sore throat, difficulty swallowing, and swollen neck.
- Inhalation Anthrax (Lung Infection)
The deadliest form of anthrax, it starts developing after breathing in spores. It is characterised by flu-like symptoms before it gets worse. Symptoms include:
- Sore throat, fatigue, muscle aches, and mild fever.
- Chest discomfort, painful swallowing, and shortness of breath.
- High fever, coughing up blood, difficulty breathing, and shock.
- In severe cases, it can lead to meningitis, a life-threatening brain infection.
- Injection Anthrax (Drug-Related Infection)
Rare and mainly reported in Europe, this one occurs from injecting contaminated drugs. Symptoms include:
- Redness and severe swelling at the injection site.
- Shock and multiple organ failure.
- Meningitis in severe cases.
Early diagnosis and treatment are key, as some forms of anthrax can be fatal without treatment.
How to Diagnose Anthrax: Tests and Procedures
Diagnosis starts with a thorough examination of symptoms and exposure risk. Doctors will rule out common illnesses like flu or pneumonia before testing for anthrax. Depending on the type of anthrax suspected, different tests will be used.
The key tests for anthrax include:
- Skin Testing – A fluid sample from the suspicious sore or a small tissue biopsy is sent to the lab to test for Bacillus anthracis.
- Blood Tests – Blood is drawn to check for anthrax bacteria.
- Chest X-ray or Computed Tomography (CT) Scan – Imaging to diagnose inhalation anthrax by looking at the lungs.
- Stool Testing – If gastrointestinal anthrax is suspected, a stool sample is checked for anthrax bacteria.
- Spinal Tap (Lumbar Puncture) – If systemic anthrax is suspected, doctors check for meningitis.
Early diagnosis is key as it allows for prompt treatment and reduces the risk of complications.
How is Anthrax Treated: Medical Solutions
Timely treatment is key to curing anthrax; the earlier, the better. Following are some of the common treatment methods:
- Antibiotics: The First Line of Defence
Anthrax is treated with antibiotics, either orally, through injection or IV (intravenous) drip. The type of antibiotic used depends on the method of exposure, the strain of anthrax, and the patient’s overall health.
Commonly used antibiotics are ciprofloxacin (Cipro®) and doxycycline (Doryx®), up to 60 days of treatment.
- Antitoxins: Counteracting the Bacteria’s Toxins
In severe cases, the bacteria release toxins into the body. Injectable antitoxins will neutralise those toxins and prevent further damage. Antibiotics are given along with antitoxin therapy for better outcomes.
- Anthrax Vaccine: Preventive and Post-Exposure Use
The BioThrax® vaccine is used for prevention but can also be part of post-exposure treatment. It’s given in 3 doses over 4 weeks, along with 60 days of antibiotics.
If you suspect anthrax exposure, seek medical attention right away. Early treatment reduces complications and increases the survival rate.
What are the Risk Factors for Anthrax?
Some groups of people are at a higher risk of getting anthrax due to their job or environment. They include:
- Occupational Risk Groups
- Farmers and Livestock Handlers – People working with animals in anthrax-risk areas.
- Veterinarians – Dealing with infected animals or animal products.
- Laboratory Workers – Handling Bacillus anthracis in a controlled environment.
- Wool Mill, Tannery, and Slaughterhouse Workers – Processing animal hides, wool or meat.
- Drum Makers – Using untreated animal hides for drum making.
- Military Personnel and Travellers
Military deployed to high-risk areas and travellers visiting anthrax-affected countries are more exposed.
- Heroin Users
Injecting illegal drugs, especially heroin, increases the risk of injection anthrax, a rare but deadly infection in some areas.
Knowing these risk factors helps you take preventive measures, especially in high-risk jobs or areas.
What are the Long-Term Effects of Anthrax Exposure?
Anthrax is a serious illness which, if left untreated, can be life-threatening. The severity of complications depends on the type of anthrax contracted, and some types are more deadly than others.
Following are some of the long-term effects of anthrax exposure:
- Sepsis and Organ Failure
When anthrax gets into the bloodstream, it can cause sepsis, a condition where the body’s immune system overreacts to the infection. This can cause widespread inflammation, organ failure and, in severe cases, death.
- Hemorrhagic Meningitis
In some cases, anthrax causes meningitis, leading to severe brain and spinal cord inflammation. This can cause internal bleeding, coma or fatal neurological damage.
- Survival Rates by Anthrax Type
- Cutaneous Anthrax – With treatment, almost all patients recover. Without treatment, the fatality rate is 20%.
- Gastrointestinal Anthrax – With treatment, 60% survive; without treatment, more than half of the infected don’t survive.
- Inhalation Anthrax – The deadliest form, 55% survive with treatment, and 15% without it.
Early detection and treatment make all the difference, so get medical attention as soon as you notice the symptoms.
How to Prevent Anthrax Infection?
Preventing anthrax requires a combination of a vaccine, antibiotics, and avoiding contact with infected animals or contaminated materials. Individuals at high risk must take the following preventive measures:
- Post-Exposure Treatment
If you’ve been exposed to anthrax spores, get medical help ASAP. The recommended post-exposure treatment is:
- 60-day antibiotic treatment with ciprofloxacin, doxycycline or levofloxacin. These are approved for adults and children.
- 3-dose anthrax vaccine series to boost your immunity.
- Monoclonal antibody treatment with raxibacumab or obiltoxaximab in some cases to neutralise anthrax toxins.
- Anthrax Vaccine for High-Risk Individuals
The anthrax vaccine is not for the general public but is available for those at high risk, including:
- Military personnel
- Lab researchers working with anthrax
- Certain workers handling animal products
The vaccine doesn’t contain live bacteria and can’t give you anthrax, but it may cause soreness at the injection site or, in rare cases, allergic reactions.
- Avoid Contact with Infected Animals
If you live in or are travelling to areas where anthrax is common:
- Don’t touch livestock and untreated animal hides, fur or wool.
- Don’t eat undercooked meat from animals that may be infected.
Even in developed countries, proper handling of imported animal products and carcasses is essential to avoid accidental exposure.
FAQs About Anthrax
- What kills anthrax?
Anthrax is treated with antibiotics that target the bacteria, while antitoxins help remove the toxins released into the body. Depending on the severity, treatment can be given in or outside a hospital.
- Is anthrax a virus?
No, anthrax is caused by the bacterium Bacillus anthracis, not a virus.
- How can anthrax be prevented?
Wear nitrile or vinyl gloves when handling animals or contaminated materials. Use eye, face, and respiratory protection in areas with infected animals or rodents.
- Which gender is most affected by anthrax?
Men are more commonly affected, with studies showing 76.3% of cases occurring in males, mainly in the 30–59 age group.
- Can anthrax multiply?
Yes, anthrax spores can survive for years in the environment. Once inside a host, they activate, multiply, and spread, causing infection.
Conclusion
Anthrax is a serious bacterial infection affecting animals but can also affect humans through inhalation, ingestion or skin exposure. Most cases are treatable with antibiotics, but inhalation anthrax is severe and requires proper and timely treatment for favourable outcomes.
If you are a medical student or NEET PG aspirant, then it’s essential to know about infectious diseases like anthrax to cover your syllabus and future diagnoses. At DocTutorials, you will find a comprehensive collection of medical topics, video lectures by experts, question banks, test series, and guidance to help you master your subjects and ace the exams. Check out our NEET PG courses now and take your medical preparation to the next level!
Latest Blogs
-

NEET PG Exam 2025- Date, Pattern, Marking Scheme, Subject Wise Weightage, and Exam Mode
NEET PG Exam 2025 is the ultimate gateway for medical graduates aspiring to pursue postgraduate courses in medicine, including MD,…
-

INI CET Exam 2025: Your Roadmap to Success – Key Topics, Strategies, and Lessons from Last Year’s Papers
The INI CET exam is more than just a test; it’s a significant milestone for many medical students aiming to…
-

INI CET Exam Success: Previous Year Question Papers & Ultimate Guide – INI CET PYQ
One can feel overwhelmed while preparing for the INI CET (Institute of National Importance Combined Entrance Test). A vast syllabus,…




