Pectus Excavatum | Causes, Symptoms, Diagnosis & Treatment
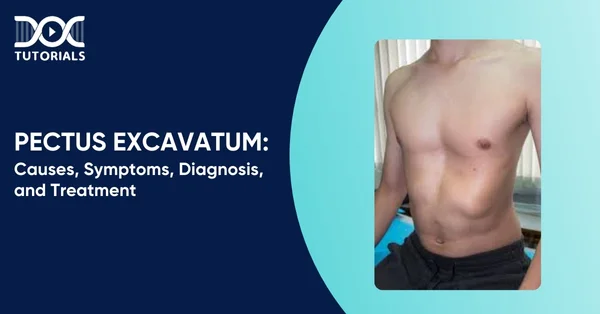
Pectus excavatum, or funnel chest, is a deformity in the chest that causes the breastbone to push inwards, resulting in the ribs growing in an irregular formation. It is the most common chest wall abnormality with a prevalence of approximately 1 in 300–400 births.
Although mild deformities are usually not an issue, more severe deformities can impair breathing, cardiac function, and self-esteem. It is usually diagnosed in adolescence and is treated, ranging from observation to corrective surgery, depending on the severity of the deformity.
Learning about this condition is crucial for medical students preparing for the NEET PG exam. Keep reading for a detailed insight into pectus excavatum, its causes, symptoms, diagnosis, and treatment.
What is Pectus Excavatum?
Pectus excavatum is a congenital chest wall deformity where the breastbone (sternum) grows inward instead of outward. This abnormal growth creates a dent or depression in the middle of the chest. In most cases, 4-5 ribs on each side pull the sternum inward and reduce the space in the chest cavity.
It is also known as a funnel chest or sunken chest. Some people have a slight dip, while others have a deep scooped-out appearance as the sternum sinks in further with age. Although it’s present at birth, the condition becomes more noticeable during adolescence when the chest starts developing.
What Causes Pectus Excavatum?
The causes of pectus excavatum are not yet fully known. However, researchers speculate it may be related to abnormal development of cartilage, the flexible tissue that connects the ribs to the breastbone. When this cartilage grows unevenly, it can pull the sternum inward and create a sunken appearance.
In some cases, it’s associated with connective tissue disorders, such as Marfan syndrome or Ehlers-Danlos syndrome, where structural abnormalities in connective tissues lead to changes in the chest wall.
What are the Risk Factors of Pectus Excavatum?
The exact cause of pectus excavatum is still unknown. However, some of the potential risk factors are listed below:
- Family History: If there is a family history of pectus excavatum, individuals are more likely to develop it.
- Connective Tissue Disorders: Marfan syndrome, Ehlers-Danlos syndrome, and osteogenesis imperfecta are conditions that affect cartilage growth and can lead to chest wall deformities.
- Genetic Syndromes: People with Noonan syndrome and Turner syndrome are also at higher risk of pectus excavatum.
What are the Symptoms of Pectus Excavatum?
Pectus excavatum can cause a mix of physical and emotional symptoms. Some people may only notice a change in chest shape, while others may experience more serious effects as the chest wall presses on the heart and lungs.
- Physical Symptoms
Some of the common physical pectus excavatum symptoms include:
- Shortness of breath during exercise
- Lesser stamina
- Fatigue with minimal exertion
- Chest pain or tightness
- Pounding, fluttering or racing heart (palpitations)
- Irregular heartbeat
- High-pitched wheeze during exercise (stridor)
- Dizziness or fainting
- Frequent upper respiratory infections
- Loss of endurance that worsens over time
- Psychological Symptoms
This sunken chest condition can significantly affect mental health as well. Many people, especially teenagers, often experience the following symptoms:
- Low self-esteem
- Issues with body image
- Embarrassment about the chest appearance
- Social withdrawal or anxiety
- Depression in severe cases
- Constant stress about appearance
How is a Pectus Excavatum Diagnosed?
Diagnosing pectus excavatum usually begins with a simple physical examination, especially during adolescence when the condition becomes more noticeable. If the chest deformity is significant, doctors may recommend tests to check if it’s affecting the heart or lungs.
Diagnosis of pectus excavatum usually begins with a basic physical examination, particularly when a child reaches their teenage years and the condition becomes more noticeable. If the chest abnormality is severe, doctors may recommend tests to determine whether it is damaging the heart or the lungs.
Some of the standard diagnostic tests include:
- Chest X-ray: Reveals the severity of the depression of the breastbone and whether the heart is displaced to one side, usually the left.
- CT (computed tomography) or MRI (magnetic resonance imaging) Scans: These provide detailed images to evaluate how severe the deformity is and whether the heart or lungs are being compressed.
- Electrocardiogram (EKG): For checking the heart’s rhythm and electrical activity. It can also be used to detect unusual heartbeats or electrical signal problems.
- Echocardiogram: This test is useful for checking if the chest wall is impacting the heart’s movement or blood flow.
- Pulmonary Function Tests (PFTs): These tests gauge the amount of air the lungs can hold and how rapidly air moves in and out, to see if the lungs have collapsed.
- Cardiopulmonary Exercise Testing: It measures how the heart and lungs perform during exercise — typically on a treadmill or stationary bike — to determine endurance and oxygen consumption.
These tests help doctors determine whether treatment is necessary and how the chest deformity may be impacting overall health.
What are the Treatment Options for Pectus Excavatum?
Surgery is the main treatment for moderate to severe pectus excavatum, especially when it causes physical or emotional symptoms. The ideal age for surgery is usually between 10 and 14 years, when the chest wall is still flexible. A few of the surgical options involve:
- Nuss Procedure (Minimally Invasive)
- Step 1: Two small incisions are made on either side of the chest.
- Step 2: A small camera is inserted for visualisation.
- Step 3: A curved steel bar is placed under the sternum and flipped to push it outward.
- Step 4: The bar is attached to the chest wall and left in place for several years.
- Step 5: It is removed in a simple outpatient procedure later.
- Ravitch Procedure (Open Surgery)
- Step 1: A larger incision is made on the front of the chest.
- Step 2: Overgrown cartilage is removed to allow proper sternum positioning.
- Step 3: The sternum is pulled forward to relieve pressure on the heart and lungs.
- Step 4: A small metal bar or plate with screws is used to hold it in place.
- Step 5: Within 6-12 months, the bar is removed. Plates, if used, are not removed.
A few of the benefits of these surgeries are listed below:
- Improves heart and lung function by decompressing
- Improves chest appearance
- Relieves psychological distress associated with the condition
A doctor will determine which procedure is best for the patient based on age, chest flexibility and symptom severity.
What are the Complications of Pectus Excavatum?
Pectus excavatum can have both physical and surgical complications. Although safe, the condition itself can affect heart and lung function, and surgical correction can cause certain complications.
- Complications Related to the Condition
- Reduced exercise tolerance due to limited heart and lung expansion
- Compression of the heart, affecting blood flow
- Mitral valve prolapse, a condition where the heart valve leaks, is sometimes caused by chest wall pressure.
- Possible Surgical Complications
- Pneumothorax (collapsed lung)
- Bleeding during or after surgery
- Pleural effusion – fluid around the lungs
- Infection at the surgical site
- Chest bar displacement – the bar may move from its original position
- Recurrence of pectus excavatum after bar removal
- Injury to nearby organs or tissues during the procedure
- Chronic chest pain after surgery
FAQs About Pectus Excavatum
1. Does pectus excavatum get worse with age?
Yes. Symptoms may worsen over time as the chest becomes less flexible and the pressure on the heart and lungs increases with age.
2. Can pectus excavatum be prevented?
No. Since the exact cause is unknown, there’s currently no way to prevent it.
3. What is the main cause of pectus excavatum?
The exact cause is not known yet, but it’s linked to abnormal growth of the cartilage that connects the ribs to the sternum. Genetics may also play a role.
4. What deficiency causes pectus excavatum?
Pectus excavatum is not caused by a deficiency, but it’s more common in people with connective tissue disorders like Marfan syndrome and Ehlers-Danlos syndrome.
5. Is pectus excavatum curable?
Yes, with the help of surgery, the chest wall deformity can improve both physical function and appearance.
Conclusion
Pectus excavatum is a chest deformity that affects how your body functions and how you feel about yourself. Whether you’re facing breathlessness, chest pain, or low confidence, it’s essential to seek help. The earlier it is diagnosed, the faster it can be managed and treated. At DocTutorials, you’ll find complete resources for medical concepts—plus video lectures from experts, well-structured question banks, test series, and guidance for the NEET PG exam. Check out our NEET PG course and take the next step in your exam preparation today!
Latest Blogs
-

NEET SS Exam 2024: Analysis, Key Dates, Counselling
The NEET SS 2024 exam kicked off on March 29, 2025. Over two days and two slots, candidates across 13…
-
NEET PG Registration 2025: An Essential Guide For Exam Prep
The NEET PG registration, which is conducted online, is a crucial step in the exam process. Filling out the NEET…
-
NEET PG Syllabus 2026: A Must-Have Complete Guide for Exam Success
The NEET PG Syllabus acts as one of the foundation stones for aspiring postgraduate medical students like you who are…




