Kwashiorkor: Symptoms, Causes, Treatment, and Prevention
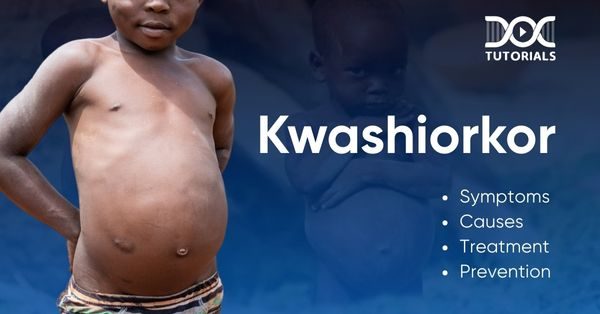
Kwashiorkor is a severe but rare form of malnutrition caused by prolonged protein deficiency that mostly affects children in areas where food is scarce. It results in swelling, a big belly, and skin changes. If left untreated, it can lead to stunted growth, organ failure, and even death.
This guide breaks down kwashiorkor in a simple and comprehensive way for medical aspirants and healthcare professionals to understand its impact and solutions. Learning this can make a huge difference in patient care and global health.
What is Kwashiorkor?
Kwashiorkor is a type of severe protein-energy undernutrition (PEU) caused by extreme protein deficiency. Unlike other types of malnutrition, kwashiorkor causes fluid retention (oedema), which leads to swelling in the hands, feet, face, and belly.
Kwashiorkor is caused by a prolonged absence of protein and a deficiency of micronutrients. Unlike Marasmus, which causes extreme weight loss, Kwashiorkor and Marasmus are different in symptoms. Kwashiorkor causes swelling due to fluid retention.
Other names for Kwashiorkor are protein malnutrition and malignant malnutrition. Recognising symptoms of Kwashiorkor early is crucial as untreated cases can lead to severe complications and even death.
Causes of Kwashiorkor
The exact cause of kwashiorkor is still unknown, but severe protein deficiency is the main factor. Some researchers have noted cases where increasing dietary protein alone did not prevent or reverse the condition, so there must be other factors as well.
Primary Causes of Kwashiorkor
- Low-Protein Diet
Kwashiorkor is caused by a diet consisting mainly of carbohydrates with little to no protein. In high-risk areas like parts of Africa, Central America, and Southeast Asia, staple foods like rice, corn, and starchy vegetables are the only available options. Protein-rich foods are scarce, especially in rural farming communities.
- Weaning Without Proper Nutrition
The word “kwashiorkor” comes from the Ga language of Ghana and means “the sickness the baby develops when the new baby arrives.” It describes how toddlers are often weaned to make way for newborns but without a proper replacement diet. This lack of protein and nutrients leads to kwashiorkor symptoms like severe swelling and malnutrition.
Other Contributing Factors
- Micronutrient Deficiencies – Lack of essential vitamins and minerals makes the body unable to process food properly.
- Aflatoxins – Mould toxins found in crops, especially in hot and humid climates, may contribute to kwashiorkor symptoms.
- Infections and Diseases – Measles, malaria, and HIV can worsen malnutrition, making the body more vulnerable.
- Environmental Stress—War, famine, and natural disasters can disrupt food supplies and increase the number of cases of kwashiorkor in affected areas.
Knowing these causes will help in coming up with effective prevention strategies, especially in high-risk communities.
Symptoms of Kwashiorkor
Kwashiorkor mainly affects children in protein-deficient regions such as sub-Saharan Africa, where people have a limited supply of food. Recognising kwashiorkor symptoms early is important for timely action.
Visible Symptoms of Kwashiorkor
- Oedema (Swelling): Fluid retention causes puffiness, especially in the feet, ankles, and belly. A bloated stomach is common due to fluid accumulation in the abdominal cavity (ascites).
- Skin and Hair Changes: Skin becomes dry and flaky or develops red, scaly patches (dermatitis). Hair loses its natural colour, turns rusty, becomes brittle, or falls out.
- Muscle and Growth Issues: Children with kwashiorkor lose muscle mass. Their limbs appear thin while subcutaneous fat remains. Stunted growth is a common feature in young children.
Internal and Systemic Symptoms
- Weakened Immune System: A damaged immune system leads to frequent and severe infections.
- Fatigue and Irritability: Persistent tiredness and mood swings are common.
- Digestive Issues: Chronic diarrhoea and loss of appetite add to malnutrition.
- Liver Complications: Enlarged liver (fatty liver) is seen in severe cases.
- Dehydration: Lack of fluids worsens overall health and leads to more complications.
Diagnosis of Kwashiorkor
Kwashiorkor is diagnosed with a physical examination followed by laboratory tests to examine nutritional deficiencies.
Physical Examination
First, a doctor will look for visible signs like oedema (swelling in the feet, ankles, and belly) and an enlarged liver (hepatomegaly). Since kwashiorkor is caused by severe protein deficiency, muscle wasting and skin changes may also be present.
Blood and Urine Tests
To assess the severity of malnutrition, the doctor will do blood and urine tests for:
- Blood and sugar levels to check for deficiencies.
- Blood urea nitrogen (BUN) and creatinine levels to check kidney function and muscle breakdown.
- Potassium levels to check electrolyte imbalance.
- Complete blood count (CBC) to check overall health and immune response.
- Arterial blood gas tests to check blood acidity and oxygen levels.
- Urinalysis to check for malnutrition and organ dysfunction.
Since kwashiorkor and marasmus symptoms are similar, these tests will help distinguish between the two and get the right treatment.
Treatment Options for Kwashiorkor
Early intervention is key to treating kwashiorkor; delaying treatment can lead to complications. The World Health Organization (WHO) has a structured approach to managing severe malnutrition, so recovery is gradual and safe.
Critical Steps in Kwashiorkor Treatment
- Managing Hypoglycemia and Hypothermia
Malnourished bodies can’t regulate blood sugar and temperature. Glucose is introduced in small amounts to prevent kwashiorkor from getting worse. Patients are kept warm to avoid hypothermia complications.
- Rehydration with RESOMAL (Rehydration Solution for Malnutrition)
Dehydration is common in kwashiorkor, so rehydration is essential. RESOMAL is designed to restore electrolytes and prevent imbalances that can cause serious complications.
- Correcting Electrolyte Imbalances
Refeeding can cause metabolic shifts. Medical teams adjust sodium, potassium, and other electrolytes before food is introduced.
- Addressing Infections
Weakened immune systems make people prone to infections. Antibiotics are given to prevent serious illness, and vitamin and mineral deficiencies are corrected before food is introduced to support recovery.
- Micronutrient Supplementation
Severe malnutrition causes vitamin and mineral deficiencies that affect growth and cognitive function. Supplements are given to correct these imbalances.
- Slow and Controlled Refeeding
Refeeding too fast can cause metabolic changes. Protein is introduced slowly to allow the body to adjust and prevent refeeding syndrome.
- Encouraging Catch-Up Growth
Once stable, children are given higher-calorie meals, sometimes up to 140% of their needs. This phase can take several weeks to support weight gain and physical recovery.
- Providing Emotional and Cognitive Stimulation
Malnutrition can affect neurological development and make children withdrawn. Activities and emotional support help restore normal cognitive and social skills.
- Long-Term Nutritional Education and Support
Before discharge, families are taught about proper nutrition, breastfeeding, and hygiene. Immunisations may also be given to prevent future illnesses.
Prevention of Kwashiorkor
Preventing kwashiorkor begins with nutrition, awareness, and healthcare. Address the root causes and eradicate this severe form of malnutrition.
1. Education and Awareness
The number one cause of kwashiorkor’s prevalence is the lack of knowledge about its symptoms and basic nutrition. Educate the community about a balanced diet, breastfeeding, and children’s nutrition needs to prevent malnutrition early on.
2. Improving Nutritional Support
Kwashiorkor is deeply rooted in food insecurity. WHO promotes sustainable farming and introduces native crops rich in protein and micronutrients. Locally made formula using skim milk and peanuts is accessible nutrition in at-risk areas.
3. Strengthening Disease Control
Infections and chronic illnesses will weaken immunity, increase nutrient loss, and lead to kwashiorkor in a vulnerable population. Immunisation, better sanitation, and access to clean water will reduce malnutrition cases.
Complications of Kwashiorkor
If left untreated, kwashiorkor can cause serious and life-threatening complications across many systems.
1. Liver and Metabolic Issues
Enlarged liver (hepatomegaly) from fat accumulation. Metabolic derangements, insulin resistance, electrolyte imbalance, and hypothermia will further weaken the body.
2. Immune System Failure
Severe protein deficiency will lead to loss of immune function, and infections will be more frequent and severe. A septic shock from bacterial infections can be fatal.
3. Digestive and Endocrine Disorders
Kwashiorkor will affect digestion and cause pancreatic atrophy, bacterial overgrowth, and glucose intolerance. Endocrine problems will occur as insulin drops and growth hormone increases, leading to developmental delays.
4. Cardiovascular and Systemic Collapse
In extreme cases, cardiovascular failure (hypovolemic shock) will occur from fluid imbalance. Impaired cellular function and electrolyte imbalance will add to organ dysfunction.
Kwashiorkor vs. Marasmus: Key Differences Explained
Kwashiorkor and marasmus are both forms of protein-energy malnutrition, but they are different in many ways:
| Reasons | Kwashiorkor | Marasmus |
| Cause | Primarily due to severe protein deficiency despite adequate calories. | From total micronutrient deficiency (proteins, carbohydrates and fats). |
| Age of Onset | More common in older children. | Usually in infants and very young children. |
| Symptoms | Characterised by oedema (swelling due to fluid retention), a distended abdomen, and changes in hair colour and texture. | Severe muscle and fat wasting, hence very emaciated with no oedema. |
| Physical Appearance | Children look puffy or swollen due to oedema. | Children look extremely thin and frail with prominent bones. |
| Liver Function | Often with an enlarged liver (hepatomegaly). | No liver enlargement. |
| Adaptation to Starvation | Considered a maladaptive response to protein deficiency. | Body’s adaptive response to overall calorie deprivation. |
Understanding these distinctions is crucial for accurate diagnosis and appropriate treatment of these malnutrition disorders.
FAQs about Kwashiorkor
1. What causes kwashiorkor?
Kwashiorkor is caused by severe protein deficiency, but other factors can also be involved, as protein alone doesn’t always prevent or cure it.
2. Why is kwashiorkor called “Red Boy”?
In some African dialects, kwashiorkor means “deposed child” (children weaned off breast milk). In another dialect, it means “red boy” due to the reddish-orange hair discolouration in affected children.
3. How is kwashiorkor treated?
High-protein diets can be obtained from animal sources (dried skimmed milk) or plant sources (soy protein). Proper medical supervision is key.
4. What is another name for kwashiorkor?
It is also called oedematous malnutrition due to the swelling (oedema) caused by fluid retention.
5. What are the main causes of kwashiorkor?
- A diet lacking protein-rich foods (mainly rice, maise or cassava).
- Infections like measles.
- Weaned off breast milk too soon.
- Childhood poverty or loss of caregivers.
6. What are the symptoms of kwashiorkor?
Early signs are fatigue, irritability, and slow growth. As it worsens, it causes muscle loss, swelling (oedema), a distended belly, weak immunity, and skin or hair changes.
Conclusion
Kwashiorkor is a severe form of malnutrition which can be life-threatening if not treated. Early intervention is necessary to prevent long-term health effects, especially in children. However, treatment has to be done carefully—increasing protein intake may not be enough and can even be harmful without proper medical supervision. If you are a medical student, DocTutorials provides a wealth of resources on topics like kwashiorkor, high-quality video lectures, question banks, test series, and expert guidance to help you master key medical concepts. Join DocTutorials’ NEET PG course to excel in your medical career.
Latest Blogs
-

NEET PG Exam 2025- Date, Pattern, Marking Scheme, Subject Wise Weightage, and Exam Mode
NEET PG Exam 2025 is the ultimate gateway for medical graduates aspiring to pursue postgraduate courses in medicine, including MD,…
-

INI CET Exam 2025: Your Roadmap to Success – Key Topics, Strategies, and Lessons from Last Year’s Papers
The INI CET exam is more than just a test; it’s a significant milestone for many medical students aiming to…
-

INI CET Exam Success: Previous Year Question Papers & Ultimate Guide – INI CET PYQ
One can feel overwhelmed while preparing for the INI CET (Institute of National Importance Combined Entrance Test). A vast syllabus,…




